Scientists have discovered how tumors secretly drain the energy from T cells—the immune system's main cancer fighters—and how blocking that process can bring them back to life.
The team found that cancer cells use a little-known molecular signal to push T cells into exhaustion, making them stop attacking. By interrupting this harmful signal, researchers were able to keep T cells active, help them infiltrate tumors, and boost the effects of existing immunotherapies.
Tumors Hijack Immune Signaling to Exhaust T Cells
A new study has identified a molecular signal that cancer cells use to drain energy from the T cells designed to eliminate them, and it also reveals how shutting down this signal may help restore the body's immune defenses. The research, led by scientists at Weill Cornell Medicine and published today (November 17) in Nature Immunology, shows that tumors do more than hide from the immune system. They can actually shift immune cells into a state where they stop attacking.
"Our dream is to make immune-based therapies available to every patient. To overcome resistance, we must unlock the power of exhausted T cells, reviving them to destroy cancer. This discovery moves us closer to a future where the immune system itself defeats tumors," said the study's co-senior author, Dr. Taha Merghoub, Margaret and Herman Sokol Professor in Oncology Research, and professor of pharmacology at Weill Cornell Medicine.
Why Cancer Outmaneuvers Immunotherapy
Immunotherapy has reshaped cancer treatment in recent years by training the body's own immune system to recognize and fight tumors. Despite this progress, many people fail to respond to treatment, or their initial response weakens as their T cells lose stamina and slip into exhaustion.
"Our findings reveal a completely new way that tumors suppress the immune system," said co-senior author Dr. Jedd Wolchok, the Meyer Director of the Sandra and Edward Meyer Cancer Center, professor of medicine at Weill Cornell and an oncologist at NewYork-Presbyterian/Weill Cornell Medical Center. "By blocking this pathway, we can help exhausted T cells recover their strength and make existing immunotherapies work better for more patients."
Understanding T Cell Exhaustion Mechanisms
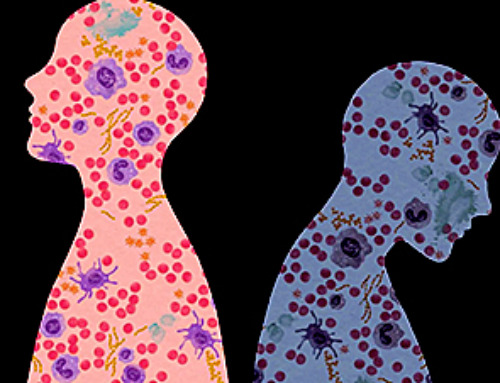
T cell exhaustion develops when the immune system is exposed to long-lasting infections or persistent tumor activity. In this weakened state, T cells can still recognize threats, but they no longer act on them.
"So, they're primed, but they're no longer killing," said Dr. Merghoub, who is also deputy director of the Meyer Cancer Center and co-director of the Parker Institute of Cancer Immunotherapy at Weill Cornell. "Although such cellular surrender may seem counterproductive, it serves as a brake to protect against out-of-control inflammation and sepsis," Dr. Merghoub said.
Previous studies have shown that a protein called PD1, found on the surface of T cells, is central to this braking process. Drugs known as checkpoint inhibitors target PD1 and have been highly effective at restoring T cell activity against cancers such as melanoma.
Hunting for New Immune 'Brakes' Beyond PD1
The researchers started out investigating whether CD47 molecules present on cancer cells contributed to T cell exhaustion. Previous studies showed that tumors can use CD47 to instruct the immune cells that normally engulf invaders to stand down—a skill that prompted its nickname as a "don't eat me signal."
But they were surprised to discover that CD47 has another function on the surface of T cells. "When T cells are activated, they express CD47. And when they get exhausted, they increase CD47 to very high levels," Dr. Merghoub said.
The Missing Partner in Suppressing T Cells
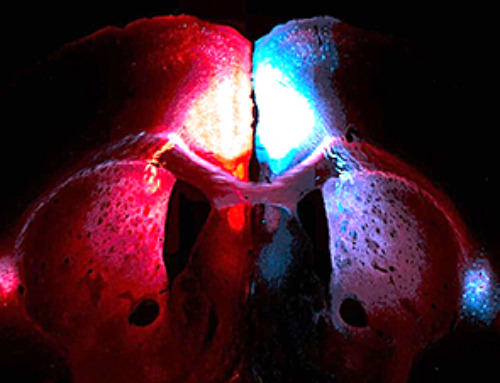
Their experiments found that mice lacking CD47 had delayed tumor growth. This suggested CD47 on the animal's immune cells, not the CD47 on the cancer cells, was causing exhaustion. They suspected that eliminating CD47 on T cells could be beneficial. When tested in mice with melanoma, T cells lacking CD47 were better at fighting the cancer than T cells, which had CD47 intact.
The researchers turned their attention to how the cancer cells coopted T-cell CD47 to promote exhaustion. They focused on a large protein called thrombospondin-1 that interacts with CD47 and is produced by metastatic cancer cells. When they tested mice lacking thrombospondin-1, they found that T cells were less exhausted. "That was the real eureka moment," said Dr. Merghoub. "It showed us that CD47 and thrombospondin are clearly key players because eliminating either one gives you the same effect."
Disrupting the CD47–TSP-1 Connection to Restore Immunity
To better understand what was happening, the researchers used the TAX2 peptide that was designed to selectively disrupt the interaction between CD47 and thrombospondin-1 in their mouse tumor models. Their suspicions were confirmed: TAX2 preserved T-cell function and slowed down tumor progression in mice with melanoma or colorectal tumors.
The T cells in treated mice stayed more active, produced more immune boosting cytokines and were better at infiltrating tumors. In addition, TAX2 worked in synergy with PD-1 immunotherapy in controlling colorectal tumor growth.
Dual-Targeting Strategy Could Unlock Stronger Cancer Therapies
"We used the TAX2 peptide as a proof-of-concept to confirm that disrupting the crosstalk between TSP-1 and CD47 prevents T cell exhaustion in mice with tumors," said Dr. Chien-Huan (Gil) Weng, an instructor in pharmacology and the study's lead author. "Next, we plan to study both upstream and downstream modulators that regulate the TSP-1:CD47 pathway and develop means to selectively, effectively and safely disrupt this pathway to improve T cell-based cancer immunotherapy."
Interfering with this interaction has the potential to serve as a useful treatment strategy on its own, and it may also help maintain the strength of tumor-targeting T cells in patients who could otherwise become resistant to current T cell-based immune checkpoint therapies. Dr. Merghoub noted that results from preclinical tumor models are especially encouraging, as they show that blocking both PD1 and CD47 leads to T cells that are far better at destroying cancer cells. "We plan to explore this therapeutic angle."
Reference: 17 November 2025, Nature Immunology.
DOI: 10.1038/s41590-025-02321-5
This research was funded in part through the National Institutes of Health grant #R01- CA249294; National Cancer Institute, Cancer Center Support Grant P30CA008748; the Department of Defense grants W81XWH-21-1-0101 and W81XWH-20-1-0723; the Swim Across America, Ludwig Institute for Cancer Research, Ludwig Center for Cancer Immunotherapy at Memorial Sloan Kettering, Cancer Research Institute; the Parker Institute for Cancer Immunotherapy; and the Breast Cancer Research Foundation grants BCRF-22-176, BCRF-23-176.