The coronavirus disease 2019 (COVID-19) pandemic has caused several waves of infections in many world regions, so strong as to overwhelm local healthcare services. In this new situation, faced with an unknown virus, the need is to produce clinical guidelines that help recognize and manage critical COVID-19. Meanwhile, conditions such as chronic obstructive pulmonary disease (COPD) are linked to a markedly increased risk of death in community pneumonia.
A new preprint available on the bioRxiv* preprint server uses computational algorithms to tease out the interrelationships between these two conditions that cause similar outcomes. Based on protein-protein interactions (PPIs), the paper shows the presence of ten genes that overlap between the two illnesses, also shared by several other deadly and debilitating diseases.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread worldwide and has led to approximately five million deaths so far. Older adults are by far the worst affected by COVID-19, with this illness accounting for 80% of all deaths in the 65-and-above age group.
Interestingly, this age group is also at the highest risk of COPD. In this condition, found in a tenth of people over 40 years, the airflow is limited, mostly caused by chronic bronchitis or emphysema. Many genetic and environmental factors play a part in the occurrence of this disease, including irritant chemical inhalation or smoking, though only about a fifth of smokers have COPD.
While COPD patients rarely acquire COVID-19, the risk of death is much higher than non-COPD patients. Accordingly, recent recommendations have been made to update the diagnostic and treatment protocols for COPD.
Independent of COVID-19, COPD is responsible for the third-largest number of deaths in the world. Considered a polygenic condition, it renders its victims susceptible to severe disease and death following the triggering of a cytokine storm by SARS-CoV-2 infection.
The latter causes symptoms only after about five days, with death, if it occurs, taking place at an average of 14 days later, depending on the patient’s age and immunity.
However, COPD is a treatable condition, if not curable, with current therapies able to maintain a high quality of life and keep the patient safe from other respiratory illnesses. When it coexists with COVID-19, the respiratory tract suffers because of the pre-existing lung injury. Thus, severe COVID-19 is fourfold more likely in such patients.
COPD patients have higher levels of the viral entry receptor, the angiotensin-converting enzyme 2 (ACE2), as do smokers.
What did the study show?
The researchers constructed a PPI network using available data on ~5,500 COVID-19 and 296 COPD gene expression profiles to elucidate the genes involved in such complicated conditions.
They first identified 248 overlapping genes, of which ten were found to be the top common genes. These are implicated in cell-cell communication and metabolism, development, the response to stimuli, and biological regulation. These genes are mostly also involved in pathways implicated in malaria, trypanosomiasis, and inflammatory bowel disease (IBD).
The Interleukin 10 (IL 10) gene is the first common gene, or the hub gene, expressing a regulatory cytokine that modulates the inflammatory response. It is markedly upregulated in associated with the cytokine storm in severe COVID-19 patients admitted to the intensive care unit (ICU).
It is, however, low in patients with COPD who have dramatic airway inflammation. IL-10 thus serves as a marker of disease severity and is useful for monitoring treatment.
The study similarly elucidates the role of Toll-like receptor 4 (TLR4), expressed by multiple immune cells and found to be required for the initiation of inflammatory responses. When it increases excessively, hyperinflammation may set in.
The TLRs are driven by the recognition of viral RNA or dsDNA intermediate forms (called pathogen-associated molecular patterns (PAMPs). These are formed from the viral genome and recognized by pattern recognition receptors, especially the TLRs, triggering further inflammatory antiviral cascades that eventually clear the virus.
TLR4 is found to have the highest PPI with the viral spike protein compared to other TLRs. SARS-CoV-2 is found to enhance the expression of interferon-stimulated genes (ISGs) in the respiratory tract. However, the higher levels of ISG expression can cause greater ACE2 expression as well. Research shows how lung surfactants block the infection by TLR4 binding and activation.
Other hub genes include the Tumor necrosis factor (TNF), a key inflammatory mediator that is elevated in acute inflammation due to viral infection, and chronic or systemic inflammation. High TNF levels are found in patients with COPD and patients with acute COVID-19 and COPD.
Fourthly, IL6 is a potent inflammatory cytokine, with multiple actions in the inflammatory cascade. It is produced by many cell types, including epithelial airway cells and alveolar macrophages. High IL6 levels are associated with worse lung function and an accelerated rate of deterioration and skeletal muscle weakness in COPD.
IL8, also known as CXCL8, is a mediator for neutrophil tracking and is implicated in inflammatory processes, notably after viral infections. Respiratory muscle weakness in patients with COPD is traceable in part to IL8 activity, with rises in the level of this cytokine during COPD exacerbations. High CXCL8 levels are suggested to be the cause of death in severe COVID-19.
IL4 is an activator of the JAK-STAT pathway that drives inflammation and mediates hyper-responsiveness of the airways, a key COPD element.
The seventh hub gene is ICAM1, an intercellular adhesion molecule that is overproduced during early inflammation, causing the premature release of neutrophils. This molecule is elevated in COPD patients. With moderate to severe COVID-19, ICAM1 levels are high and increasing but drop in convalescence.
This may mean that these molecules are markers of COVID-19 severity. Besides, they also trigger coagulation defects. The four intracellular binding sites for SARS-CoV-2 within human cells are highly expressed in COPD patients.
The eighth hub gene is interferon-gamma (IFN-γ). This is known to be a key risk gene for COVID-19 patients with lung disease. COPD patients have a more than five times higher risk of severe COVID-19
TLR2 is the ninth hub gene, associated with a decline in lung function and evidence of inflammation in sputum, indicating its role in COPD pathogenesis and exacerbation. It is also known to recognize SARS-CoV-2 particles and may be part of the infection-pulmonary embolism pathway.
The last of the hub genes is IL18, which is thought to be tied to the abnormal inflammatory pathways in COPD. Anti-IL 18 antibodies neutralize the damage and inflammation caused by COPD in preclinical models.
News
Specially engineered antibody delivers RNA therapy to treatment-resistant tumors
Elias Quijano, PhD; Diana Martinez-Saucedo, PhD; Zaira Ianniello, PhD; and Natasha Pinto-Medici, PhD, there are 25 other contributors, most from Yale's Department of Therapeutic Radiology and from the departments of genetics, molecular biophysics and [...]
Vaccinated women face fewer cervical cancer risks
New data from Denmark shows the HPV vaccine’s powerful long-term impact, while also revealing why cervical cancer screening is still essential. A Danish study published in the journal Eurosurveillance reports that women who received the human [...]
3D-printed implant offers a potential new route to repair spinal cord injuries
A research team at RCSI University of Medicine and Health Sciences has developed a 3-D printed implant to deliver electrical stimulation to injured areas of the spinal cord, offering a potential new route to [...]
Nanocrystals Carrying Radioisotopes Offer New Hope for Cancer Treatment
The Science Scientists have developed tiny nanocrystal particles made up of isotopes of the elements lanthanum, vanadium, and oxygen for use in treating cancer. These crystals are smaller than many microbes and can carry isotopes of [...]
New Once-a-Week Shot Promises Life-Changing Relief for Parkinson’s Patients
A once-a-week shot from Australian scientists could spare people with Parkinson’s the grind of taking pills several times a day. The tiny, biodegradable gel sits under the skin and releases steady doses of two [...]
Weekly injectable drug offers hope for Parkinson’s patients
A new weekly injectable drug could transform the lives of more than eight million people living with Parkinson's disease, potentially replacing the need for multiple daily tablets. Scientists from the University of South Australia [...]
Most Plastic in the Ocean Is Invisible—And Deadly
Nanoplastics—particles smaller than a human hair—can pass through cell walls and enter the food web. New research suggest 27 million metric tons of nanoplastics are spread across just the top layer of the North [...]
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
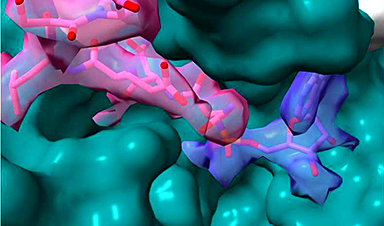
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
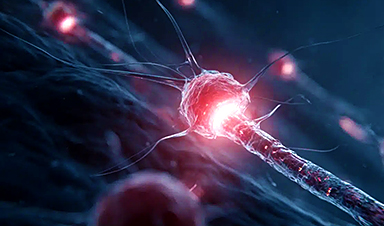
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]