Increasing drug resistance could leave us powerless to fight infections we now consider routine, and scientists are urgently searching for answers.
It was just a urinary tract infection (UTI). Helen Osment, a fundraiser from Hertfordshire, had had them before and she knew the symptoms. When she called the doctor with pain, a burning sensation and blood in her urine, they prescribed a course of antibiotics – a few days of nitrofurantoin.
But this time, her UTI didn’t go away. It got worse. The pain was bad and she started feeling feverish. As her symptoms failed to improve, she felt uncomfortable and miserable. “I think it can affect you mentally when you have one, it can make you feel quite sort of down and low,” she says.
Her doctor tried another antibiotic, trimethoprim, but the infection remained. Still feeling awful, she asked the doctor for “something stronger”. Options were limited by the fact that Osment had been deemed allergic to penicillin as a child, and this was flagged on her records (though like many who are flagged as allergic, she later turned out not to be). She was prescribed ciprofloxacin but reacted badly: she felt heart palpitations and pain in her knee, which turned out to be tendonitis, a potential side-effect of the drug. She visited a walk-in centre, where she was told to stop taking it and was put on a longer course of nitrofurantoin.
Her condition deteriorated. Feverish and in so much pain she couldn’t even pick up her baby, she ended up in A&E. “I was thinking, oh surely they’ll just give me some more antibiotics,” she says. “I didn’t realise how ill I was.” The mastitis had formed a large abscess and Osment had developed sepsis – a life-threatening condition caused by the body’s response to an infection. Luckily, this was caught early, and after being hospitalised and put on a different antibiotic intravenously, she beat the infection and recovered.
“It just goes to show that it can happen to anybody, and things can escalate very quickly,” Osment says. She now shares her story through the charity Antibiotic Research UK, to help raise awareness of antimicrobial resistance.
When Covid-19 began to spread around the globe, it was something we hadn’t seen before and we had no medicines to defend ourselves against it. But it’s not only new pathogens, like Sars-CoV-2, that pose a threat to global human health. Antimicrobial resistance means that existing bugs – ones we perhaps don’t worry too much about – are becoming resistant to the treatments we have come to take for granted, such as antibiotics. As this resistance becomes more common, we could find ourselves in a similar situation: facing infectious diseases with limited treatment options.
Our experience under Covid-19 may have given us a glimpse of that future. “It shows what the world would be like if we had resistance to all known antibiotics,” says Jessica Boname, former head of antimicrobial resistance at the UK’s Medical Research Council. “We would be in the Covid-19 world.”
The term antibiotic resistance refers specifically to bacteria becoming resistant to antibiotics. Antimicrobial resistance is a broader term that also covers other microbes such as fungi, parasites and viruses.
Today, if we get an infection, we generally expect that we can go to the doctor and get some medicine to treat it. But if the microbes causing the infection are resistant to that medicine, the infection may not go away. We might go on to try another drug, and another, and another, but if the microbes are resistant to those too, we’re back at square one. Microbes that are able to resist multiple antimicrobials are sometimes referred to as “superbugs” – and they can be very difficult to treat.
The stakes are high. If antimicrobial resistance is left to rise unchecked, we may no longer be able to knock out common infections with a simple prescription. Illnesses caused by resistant pathogens will require longer, more costly treatment. In more and more cases, we may not be able to treat a resistant infection at all.
And it’s not just routine infections that will become more dangerous as we lose more antimicrobials from our medical arsenal. Much of modern medicine is built on the assumption that we can easily fight or prevent infection. If this is no longer the case, these foundations start to crumble.
Take surgery: antibiotics are given as a preventative measure before and after many operations that have a high risk of infection, such as hip replacements, organ transplants or Caesarean sections. If we can no longer count on antimicrobials being effective, surgery will become much more risky. In some cases, it may be unviable: the risk of getting an untreatable infection will simply be too high.
For most infections, we have multiple lines of defence. If one antimicrobial doesn’t work, you try another, then another, and so on until you reach those that are held back as a last resort, to be used only in extremely limited cases so as to prevent resistance from occurring. As these antimicrobials are struck down by resistance, the obvious solution would be to make new ones. But we aren’t developing them fast enough.
According to the World Health Organisation, lack of innovation and funding is a major concern, with most new products in development showing little extra benefit and few targeting some of the most urgent infections.
Most of the antimicrobial substances that we commonly use today were found in the 40s and 50s, soon after penicillin – a “golden era” for antibiotic discovery. But in the following decades, discoveries of new antibiotics were few and far between. The low-hanging fruit had been found and scientists were getting frustrated at discovering the same compounds again and again.
In the latter part of the 20th century, a new method was adopted. Rather than screening natural compounds to search for antimicrobial substances, scientists decided to try a more targeted approach. They set out to look specifically for compounds that inhibited pathways essential to the function of bacteria. If you know a bacterium needs to create a certain enzyme to thrive, for instance, then finding a compound that inhibits the production of this enzyme could give you a promising lead for a new antimicrobial drug. Researchers turned their attention to synthetic compounds in the vast chemical libraries of research groups and pharmaceutical companies.
It’s an approach that has been successful for discovering many kinds of drugs, but it didn’t really work for antimicrobials. “They were new technologies at the time, we thought they were going to generate lots of really useful compounds,” says Mathew Upton, a professor of medical microbiology at the University of Plymouth. “And they basically generated nothing at all.”
It’s not that we didn’t find anything – promising compounds were identified – but when tested they just didn’t work in actual bacteria. And so the focus turned once again to natural substances, making the most of the tiny, living antibiotic factories in the environment all around us. These days, the way many researchers find new antibiotics is not all that dissimilar to Alexander Fleming’s observation of mould on a sample dish, albeit rather more deliberate.
The reason for searching in places so far removed from our everyday environment is that it increases the chance of finding a truly novel antibiotic compound, Upton explains. Often, researchers can find a substance with promising antibiotic properties, but once they’ve gone through the hassle of growing the microbe in the lab and purifying the compound, they find out it is the same as, or similar to, an existing antibiotic – and will therefore likely be disarmed by the same resistance mechanisms.
“If a compound is the same as something we’ve seen before, or very related to it, it’s probably not going to be worth developing, because any resistance mechanism that is already out there will undermine it as soon as we use it in the clinic,” Upton says.
But we don’t always need to look so far away from home. Upton is currently working with one compound that was found in a sample taken from the surface of human skin.
But ultimately, the things that could have the most impact are the ones we already know about – like access to clean water and sanitation, infection prevention and control measures, and improved access to existing vaccines and treatments. Similarly, if we can improve infection control measures in hospitals, we will reduce the spread of hospital-acquired infections. When people do get infections, we need to be better at treating them – using the right antimicrobials in the right patients, at the right doses. We also need to reconsider our use of antimicrobials in agriculture and the environment.
Individuals can refrain from asking for antibiotics when they have a cold and follow the instructions when they are prescribed them. Prescribers can make sure they’re sticking to stewardship guidelines.
A multitude of solutions are needed to address many different issues. Just as we have seen with the Covid-19 pandemic, we need researchers, clinicians, engineers, politicians, behavioural scientists and economists to work together across borders.
News
Nanocrystals Carrying Radioisotopes Offer New Hope for Cancer Treatment
The Science Scientists have developed tiny nanocrystal particles made up of isotopes of the elements lanthanum, vanadium, and oxygen for use in treating cancer. These crystals are smaller than many microbes and can carry isotopes of [...]
New Once-a-Week Shot Promises Life-Changing Relief for Parkinson’s Patients
A once-a-week shot from Australian scientists could spare people with Parkinson’s the grind of taking pills several times a day. The tiny, biodegradable gel sits under the skin and releases steady doses of two [...]
Weekly injectable drug offers hope for Parkinson’s patients
A new weekly injectable drug could transform the lives of more than eight million people living with Parkinson's disease, potentially replacing the need for multiple daily tablets. Scientists from the University of South Australia [...]
Most Plastic in the Ocean Is Invisible—And Deadly
Nanoplastics—particles smaller than a human hair—can pass through cell walls and enter the food web. New research suggest 27 million metric tons of nanoplastics are spread across just the top layer of the North [...]
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
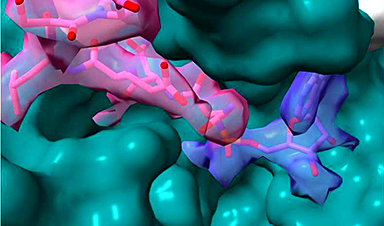
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
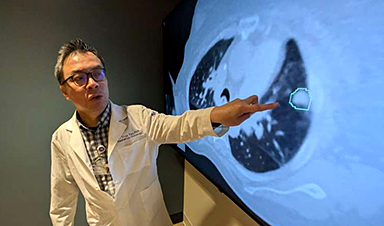
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]