Are sprays the future of COVID-19 vaccines?
That’s the hope of dozens of research groups and companies working on new kinds of inoculation. Rather than relying on injections, these use sprays or drops administered through the nose or mouth that aim to improve protection against the virus SARS-CoV-2.
This week, an inhaled version of a COVID-19 vaccine, produced by the Chinese company CanSino Biologics in Tianjin, was approved for use as a booster dose in China.
It’s one of more than 100 oral or nasal vaccines in development around the world. In theory, these vaccines could prime immune cells in the thin mucous membranes that line cavities in the nose and mouth where SARS-CoV-2 enters the body, and quickly stop the virus in its tracks — before it spreads. Vaccine developers hope that these ‘mucosal’ vaccines will prevent even mild cases of illness and block transmission to other people, achieving what’s known as sterilizing immunity. A few mucosal vaccines are already approved for other diseases, including a sprayable vaccine against influenza.
Evidence in animals supports the idea that sterilizing immunity can be induced against COVID-19, although data from humans are scant. Nature explains why mucosal vaccines might help to quash SARS-CoV-2, and what the latest findings mean.
Why might mucosal vaccines be better than conventional shots?
The COVID-19 vaccines currently in use do a good job of reducing disease severity and preventing hospitalization, but don’t block mild illness or transmission that well.
One reason is that they are injected into muscle. Intramuscular shots prompt an immune response that includes T cells, which destroy infected cells, and B cells, which produce antibodies that ‘neutralize’ pathogens — binding to them to stop them entering healthy cells. These cells and antibodies circulate through the bloodstream. But they aren’t present at high enough levels in the nose and lungs to provide rapid protection. In the time it takes for them to journey there from the bloodstream, the virus spreads, and the infected person gets ill.
Mucosal vaccines can prompt a whole-body immune response, but they can also activate immune cells in the mucosal tissue of the nose and respiratory tract. These localized cells “act as sentinels at the site of infection”, says Benjamin Goldman-Israelow, a physician-scientist at Yale School of Medicine in New Haven, Connecticut. “They can act much more quickly.”
The localized mucosal immune cells, known as tissue-resident memory T and B cells, have slightly different functions from the circulating T cells and B cells. For instance, tissue-resident memory B cells produce antibodies called secretory immunoglobulin A (IgA), which are intertwined with the layers of the respiratory tract, where they might be able to stop pathogens quickly. However, it is unclear how well secretory IgA will protect against SARS-CoV-2.
Researchers are testing mucosal vaccines as first doses for unvaccinated people and as boosters for those who have already received COVID-19 shots. Some mucosal vaccines are identical to injected vaccines, but are squirted as liquid or droplets up the nose. Others have a different composition, or are prepared differently. For instance, the mucosal vaccine developed by CanSino is the same as its injected one, but is packaged into aerosols and inhaled through the mouth with a nebulizer at one-fifth the dose of the injected version. A few mucosal vaccines in development are swallowed as pills.
How good are mucosal vaccines against other diseases?
At least nine mucosal vaccines are approved for use in people, against pathogens including poliovirus, influenza and cholera. Eight of these vaccines are taken orally, and one, against flu, is administered intranasally.
The oral polio vaccine, which induces immunity in the gut, is highly successful and comes close to achieving sterilizing immunity. In rare cases, however, this live attenuated vaccine will mutate and cause illness. For other diseases, mucosal vaccines haven’t been so successful — sometimes because the vaccine doesn’t generate a sufficiently strong immune response, and sometimes because it triggers side effects. The Swiss vaccine company Berna Biotech in Bern pulled its intranasal flu vaccine off the market in 2001, for instance, after discovering that it increased the risk of temporary facial paralysis.
A product called FluMist, a live attenuated intranasal vaccine against influenza that is approved in the United States and Europe, outperforms the intramuscular version in young children1. Adults might also find it more convenient to have a vaccine sprayed up the nose, rather than injected. But FluMist hasn’t worked as well in adults. That’s because many have had years to build up some immunity to flu viruses. Even if this immunity isn’t strong enough to prevent the disease, adults’ mucosal immune responses might still block the attenuated vaccine from infecting nasal cells, or clear it before it has a chance to do its job.
“It’s a balancing act between making sure the vaccine doesn’t cause illness, and yet replicates enough to elicit mucosal immunity in people who have had some experience with the virus,” says Kanta Subbarao, director of the World Health Organization (WHO) Collaborating Centre for Reference and Research on Influenza in Melbourne, Australia. Researchers don’t yet know if this issue might also affect COVID-19 intranasal vaccines.
Where and when might mucosal COVID-19 vaccines be available?
Around 100 mucosal COVID-19 vaccines are in development globally, according to Airfinity, a health-analytics company in London (see ‘Mucosal COVID-19 vaccines’). Around 20 of those have reached clinical trials in humans, of which at least four — in India, Iran and two in China — have completed or are undergoing phase III studies to test safety and how well they work compared to other vaccines. Iran gave its vaccine emergency approval in October 2021, and at least five million doses have been delivered to the Ministry of Health, says Ali Es-haghi, an analytical chemist at the Razi Vaccine and Serum Research Institute in Karaj, which developed the vaccine. But the institute has not yet published data on efficacy in humans. (Russia is said to have approved a mucosal vaccine for its market but has not published data, and the vaccine makers did not respond to Nature’s request for details.)
Mucosal COVID-19 vaccines
Around 100 intranasal vaccines are being investigated*, of which roughly 20 have reached trials in humans. Here are some of them.
| Developer (location) | Vaccine type | Delivery method | Status |
|---|---|---|---|
| Bharat Biotech (Hyderabad, India) | Viral vector; non-replicating | Intranasal (drops) | Company says two phase III studies completed, unpublished. Data submitted to regulators in India. |
| CanSino Biologics (Tianjin, China) | Viral vector; non-replicating (Aerosolized version of approved intramuscular vaccine) | Inhaled through nose and mouth | Approved by Chinese regulators. |
| Beijing Wantai Biological Pharmacy (Beijing) | Live attenuated | Intranasal (spray) | Phase III study under way in 40,000 people. |
| Razi Vaccine and Serum Research Institute (Karaj, Iran) | Protein subunit | Intranasal (spray) | Received emergency authorization in Iran in October 2021; in phase III trial (status unknown). |
| Codagenix (Farmingdale, New York) and Serum Institute of India (Pune) | Live attenuated | Intranasal (drops) | Phase II/III efficacy study in 20,000 people under way at undisclosed locations in Africa; part of the World Health Organization’s Solidarity Trial Vaccines. |
| Icahn School of Medicine at Mount Sinai (New York City) and Laboratorio Avi-Mex (Mexico City, Mexico) | Viral vector; non-replicating | Intranasal (drops or spray) | Phase II study under way in 396 people in Mexico City. |
| AstraZeneca (Cambridge, UK) and University of Oxford (Oxford, UK) | Viral vector; non-replicating (adenovirus) | Intranasal (spray) | Phase I study completed (both as first dose and as booster). |
| Meissa Vaccines (Redwood City, California) | Live recombinant | Intranasal (drops or spray) | Phase I study under way (both as first dose and as booster). |
| CyanVac (Athens, Georgia) | Viral vector; live, replicating | Intranasal (spray) | Phase I study under way. |
| Center for Genetic Engineering and Biotechnology (Havana, Cuba) | Protein subunit | Intranasal (spray) | Phase II study in up to 5,000 participants in Cuba. |
Large-scale human trial data on mucosal vaccines in the United States and Europe will take another year or two. “There’s not the same sense of urgency now” compared with at the beginning of the pandemic, says Louise Blair, head of vaccines and variants at Airfinity. “We are in an abundance of vaccines. Countries at the moment seem to be satisfied with protection against hospitalization rather than infection. So funding and resources are very different, and I don’t think we’ll see the same speed of development,” she says.
In the meantime, countries must rely on intramuscular boosters to maintain immunity. Some public-health authorities are updating boosters against coronavirus variants such as Omicron, although early data suggest that these perform only slightly better than an extra dose of older vaccines. But relying solely on boosters to suppress variants “may not be the optimal approach”, says Robert Seder, chief of cellular immunology at the US National Institute of Allergy and Infectious Diseases (NIAID) in Bethesda, Maryland. “To increase protection against transmission, we may need to change the delivery” of boosters to increase mucosal responses, he says.
Can mucosal COVID-19 vaccines induce sterilizing immunity?
Preventing infection and transmission is a high bar for any vaccine. But studies of SARS-CoV-2 mucosal vaccines in animals suggest that it’s possible. For example, a study2 in mice by Goldman-Israelow and his colleagues at Yale University found that an intranasal booster (given after one dose of conventional vaccine) induced mucosal immunity and completely protected the animals from a lethal level of exposure to the coronavirus, whereas an intramuscular booster did not.
And in rhesus macaques (Macaca mulatta)3, another intranasal vaccine — which used an influenza-like virus to deliver SARS-CoV-2 RNA to cells — completely protected the animals from SARS-CoV-2 infection. Virus replication was undetectable in the monkeys’ airways and lung tissues, says Ursula Buchholz, chief of the RNA viruses section at the NIAID, who led the study. “In preclinical models, we get something that’s very close to sterilizing immunity. We’ll have to see how this translates into clinical studies,” she says.
How are researchers measuring the efficacy of mucosal vaccines in people?
There’s a quick way to predict whether an intramuscular COVID-19 vaccine will be effective: measure the neutralizing-antibody levels circulating in the blood. Higher levels generally mean better protection — something researchers have established after decades of experience with intramuscular vaccines against other pathogens.
But for mucosal vaccines that aim to induce sterilizing immunity, no clear-cut correlate exists. Many developers are measuring immune responses in the respiratory tract, including secretory IgA, other antibodies and tissue-resident memory T cells. These probably contribute to protection, but it’s unclear what levels are necessary to prevent infection and transmission. Studies of immune responses in the nose and lungs of people who have experienced a natural infection might prove informative.
Until this basic research is established, mucosal-vaccine developers must determine efficacy in other ways. The company Bharat Biotech in Hyderabad, India, for instance, measured systemic neutralizing antibodies in blood serum in its trial of an intranasal COVID-19 vaccine. If those match or exceed the antibody levels of intramuscular vaccines on the market, the trial will achieve its primary endpoint and be considered a success. But it will not determine the vaccine’s ability to prevent infection or transmission. Last month, the firm said it had sent late-stage testing data — as yet unpublished — to the country’s regulator, hoping for approval to start providing the vaccine to clinics.
CanSino tracked efficacy using a similar strategy — measuring the levels of neutralizing antibodies in blood serum and comparing them to those from existing vaccines. A phase II study of the company’s aerosolized mucosal vaccine reported in January4 that, when given as a booster, the vaccine raised serum antibody levels significantly more than did a boost from CanSino’s intramuscular vaccine. In July, the firm noted in a further report that antibody levels waned over time, but were still higher than those elicited through the intramuscular route5. The company is also measuring T cells and antibodies in saliva, but the levels of response needed to provide sterilizing immunity aren’t known.
The Chinese firm Beijing Wantai Biological Pharmacy also has a mucosal vaccine in phase III trials, but the company did not respond to Nature’s request for comment.
Another option is to conduct efficacy studies by comparing a mucosal vaccine against a placebo group. Codagenix in Farmingdale, New York, and the Serum Institute of India in Pune are taking this approach in a phase II/III study of an intranasal vaccine in 20,000 unvaccinated people, about half of whom will receive a placebo in their noses. Efficacy will be determined by comparing the number of confirmed cases in each group and measuring the rate of protection from the vaccine, says Robert Coleman, chief executive at Codagenix.
Placebo groups are getting harder to assemble as the number of people who haven’t been infected with SARS-CoV-2 or vaccinated dwindles. Such trials are also hard to justify ethically when effective vaccines are readily available. However, there are countries that have low vaccination rates and limited vaccine access, where such a trial can be conducted ethically. Codagenix’s phase II/III study is part of the WHO’s Solidarity Trial Vaccines, which brings several trials together to share one placebo group. A Codagenix spokesperson says that trials are being conducted in countries in Africa to start with, but did not disclose details. They aren’t expected to yield results until 2023. (Codagenix is also working on a trial of its intranasal vaccine as a booster, currently in phase I.)
“It’s completely possible to determine efficacy,” says Sandy Douglas, who is chief investigator of an intranasal SARS-CoV-2 vaccine being developed by the University of Oxford, UK. “It’s just a bit trickier than testing first-generation intramuscular vaccines in an infection-naive population,” he says.
News
Scientists Crack a 50-Year Tissue Mystery With Major Cancer Implications
Researchers have resolved a 50-year-old scientific mystery by identifying the molecular mechanism that allows tissues to regenerate after severe damage. The discovery could help guide future treatments aimed at reducing the risk of cancer [...]
This New Blood Test Can Detect Cancer Before Tumors Appear
A new CRISPR-powered light sensor can detect the faintest whispers of cancer in a single drop of blood. Scientists have created an advanced light-based sensor capable of identifying extremely small amounts of cancer biomarkers [...]
Blindness Breakthrough? This Snail Regrows Eyes in 30 Days
A snail that regrows its eyes may hold the genetic clues to restoring human sight. Human eyes are intricate organs that cannot regrow once damaged. Surprisingly, they share key structural features with the eyes [...]
This Is Why the Same Virus Hits People So Differently
Scientists have mapped how genetics and life experiences leave lasting epigenetic marks on immune cells. The discovery helps explain why people respond so differently to the same infections and could lead to more personalized [...]
Rejuvenating neurons restores learning and memory in mice
EPFL scientists report that briefly switching on three “reprogramming” genes in a small set of memory-trace neurons restored memory in aged mice and in mouse models of Alzheimer’s disease to level of healthy young [...]
New book from Nanoappsmedical Inc. – Global Health Care Equivalency
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
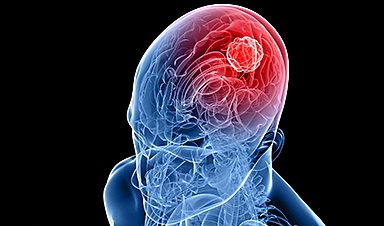
New Molecule Blocks Deadliest Brain Cancer at Its Genetic Root
Researchers have identified a molecule that disrupts a critical gene in glioblastoma. Scientists at the UVA Comprehensive Cancer Center say they have found a small molecule that can shut down a gene tied to glioblastoma, a [...]
Scientists Finally Solve a 30-Year-Old Cancer Mystery Hidden in Rye Pollen
Nearly 30 years after rye pollen molecules were shown to slow tumor growth in animals, scientists have finally determined their exact three-dimensional structures. Nearly 30 years ago, researchers noticed something surprising in rye pollen: [...]
NanoMedical Brain/Cloud Interface – Explorations and Implications. A new book from Frank Boehm
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
How lipid nanoparticles carrying vaccines release their cargo
A study from FAU has shown that lipid nanoparticles restructure their membrane significantly after being absorbed into a cell and ending up in an acidic environment. Vaccines and other medicines are often packed in [...]
New book from NanoappsMedical Inc – Molecular Manufacturing: The Future of Nanomedicine
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
A Virus Designed in the Lab Could Help Defeat Antibiotic Resistance
Scientists can now design bacteria-killing viruses from DNA, opening a faster path to fighting superbugs. Bacteriophages have been used as treatments for bacterial infections for more than a century. Interest in these viruses is rising [...]
Sleep Deprivation Triggers a Strange Brain Cleanup
When you don’t sleep enough, your brain may clean itself at the exact moment you need it to think. Most people recognize the sensation. After a night of inadequate sleep, staying focused becomes harder [...]
Lab-grown corticospinal neurons offer new models for ALS and spinal injuries
Researchers have developed a way to grow a highly specialized subset of brain nerve cells that are involved in motor neuron disease and damaged in spinal injuries. Their study, published today in eLife as the final [...]
Urgent warning over deadly ‘brain swelling’ virus amid fears it could spread globally
Airports across Asia have been put on high alert after India confirmed two cases of the deadly Nipah virus in the state of West Bengal over the past month. Thailand, Nepal and Vietnam are among the [...]
This Vaccine Stops Bird Flu Before It Reaches the Lungs
A new nasal spray vaccine could stop bird flu at the door — blocking infection, reducing spread, and helping head off the next pandemic. Since first appearing in the United States in 2014, H5N1 [...]