Novel three-drug regimen used to manage life-threatening developments.
In April 2021, a 42-year-old man reached out to Brian Hill, MD, PhD, for a second opinion after being diagnosed with hairy cell leukemia following a bone marrow biopsy at a healthcare facility in northwest Ohio.
“At the time of diagnosis, he was getting easily fatigued and couldn’t exercise,” explains Dr. Hill, Director of the Lymphoid Malignancies Program at Cleveland Clinic’s Taussig Cancer Institute. “He was experiencing a slow-moving progression of symptoms.”
Standard front-line therapy for hairy cell lymphoma –an indolent B-cell lymphoproliferative disease – is the chemotherapy medication cladribine. Dr. Hill recommended the patient begin the drug, typically administered daily for five days or via a continuous pump for seven days, but the situation quickly pivoted.
“When I met the patient for a virtual second opinion, I recommended he get vaccinated against SARS-CoV-2 before beginning treatment,” says Dr. Hill. “Within two weeks, however, he was hospitalized with COVID-19 pneumonia.”
Severe COVID-19 sends patient to ICU
The patient was admitted to his local hospital with fever and shortness of breath. He tested positive for COVID-19, and within a few days, his breathing became more labored. He was transferred to Cleveland Clinic’s main campus.
“His critical illness was exacerbated by neutropenia from his leukemia,” says Dr. Hill. “Once he was admitted to our ICU, he rapidly deteriorated.” Within a few days, the patient was intubated and put on mechanical ventilation. His oxygenation levels were so poor that he was placed in the prone position and underwent pharmacologic paralysis.”
Unfortunately, the patient’s severe COVID had severely compromised his immune system. “The only way to improve his neutrophil and white blood cell counts was to get the cancer cells out of the bone marrow,” says Dr. Hill. However, the oncology team quickly realized that the standard chemotherapy approach for hairy cell leukemia could prove detrimental.
“He would unlikely survive short-term worsening of his neutropenia caused by the administration of traditional chemotherapy with cladribine,” explains Dr. Hill.
Second-line treatment given through NG tube
After discussions with other oncologists and the patient’s critical care team, including pulmonology specialists, Dr. Hill began to administer vemurafenib, an FDA-approved tablet medication for treating melanoma that targets mutations in the BRAF gene.
Approximately 90% of hairy cell leukemia cases also have this same BRAF mutation, says Dr. Hill. Although vemurafenib is not as effective as cladribine for hairy cell leukemia, the drug has been proven to be an effective second-line treatment.
Twice a day for more than two weeks, caregivers crushed a 960-mg tablet of vemurafenib and administered it to the patient through a nasogastric tube. He also was treated with remdesivir for COVID-19.
Gradually, the patient’s neutrophil count recovered, his breathing improved and his fever abated. He was weaned off high levels of oxygen.
“His COVID finally turned the corner,” says Dr. Hill. “I give most of the credit to our medical ICU nurses, pharmacists and physicians whose great work kept him going through all this.”
Complications, more treatment and remission
During his time in the hospital, the patient suffered numerous complications, including bacteremia, ventilator-associated pneumonia. He also lost some function in his left hand from neurologic compression of his brachial plexus.
After two months in the medical ICU, the patient was transferred to a medical-surgical unit in mid-June and was later discharged from the hospital July 1. His treatment journey for hairy cell leukemia continued throughout.
“While vemurafenib is a good drug, it wasn’t good enough in his case,” says Dr. Hill. “He stopped making progress while in the hospital, so we gave him a 70% dose of cladribine.” Once discharged, the patient received a standard dosage of the monoclonal antibody medication rituximab, which was necessary due to ongoing cytopenias.
“It was a balancing act to provide enough treatment against the hairy cell leukemia, but not so much to set him back in terms of infectious complications,” explains Dr. Hill.
A year after his hairy cell leukemia diagnosis, the patient is in remission. His only residual medical deficit is impaired inflection of his left wrist, for which he is undergoing physical therapy. The patient is back at home with his family, including his wife and three children. He hopes to return to work within the next few months.
“For patients like this one with rare diseases who have atypical treatment courses, it’s important to think outside the box to get the best outcomes. Cleveland Clinic excels at that,” says Dr. Hill. “In this case, we could not wait for the patient to get better from COVID to treat the cancer. We had to address both at once.”
News
Most Plastic in the Ocean Is Invisible—And Deadly
Nanoplastics—particles smaller than a human hair—can pass through cell walls and enter the food web. New research suggest 27 million metric tons of nanoplastics are spread across just the top layer of the North [...]
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
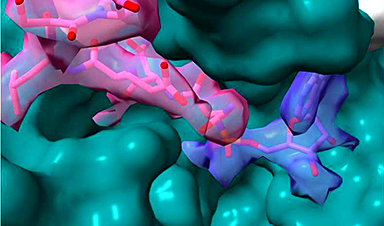
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
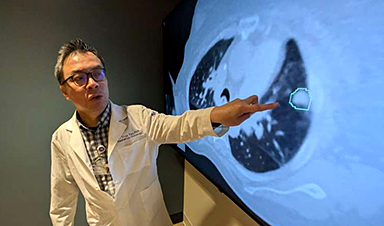
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]