Exclusive: study raises hopes that Covid-related damage to sense of smell may be more superficial than previously feared.
The virus that causes Covid-19 does not infect human brain cells, according to a study published in the journal Cell. The findings will raise hopes that the damage caused by Sars-CoV-2 might be more superficial and reversible than previously feared.
The study contradicts earlier research that suggested the virus infects neurons in the membrane that lines the upper recesses of the nose.
This membrane, called the olfactory mucosa, is where the virus first lands when it is inhaled. Within it are olfactory sensory neurons (OSNs), which are responsible for initiating smell sensations. They are tightly entwined with a kind of support cell called sustentacular cells.
In the new study, Belgian and German researchers claim that the virus infects sustentacular cells but not OSNs. “That is just a critical distinction,” said the senior author Peter Mombaerts, who directs the Max Planck Research Unit for Neurogenetics in Frankfurt, Germany. “Once you believe that olfactory neurons can be infected, there is a quick route into the olfactory bulb and then you’re in the brain already.”
The olfactory bulb, at the front of the brain, is where neural input about odours is first processed. If the virus penetrated this structure it could theoretically spread to deeper brain regions where it could do lasting damage – especially since, unlike OSNs, most neurons are not regenerated once lost.
But if the virus only infects the sustentacular cells, then the damage could be less long-lasting.
Both pathways could explain the olfactory dysfunction that afflicts an estimated half of all Covid-19 patients. In one in 10 of those, the loss or change of smell is long-term, perhaps permanent.
Mombaerts says this could be the result of support for the OSNs breaking down, even if they themselves are not infected. They may function below par, or stop functioning altogether, until the sustentacular cells regenerate.
The group has not looked at other neurological symptoms of Covid-19, such as the fatigue and “brain fog” that accompany long Covid.
Nobody doubts that the central nervous system is affected by the disease; the debate concerns whether these effects are due to the virus infecting neurons or some more indirect mechanism, such as an inflammatory response in the blood irrigating the brain – with different implications for prognosis and treatment.
The findings are likely to prove controversial because of the difficulty of studying molecular events unfolding in the moments after infection. Earlier studies made use of animal models, clusters of neural stem cells grown in a dish, and postmortem tissue taken from small numbers of Covid-19 patients. The present study is the largest in Covid-19 patients to date, and it deployed a novel technique for capturing those early events.
Laura Van Gerven, a neurosurgeon at the Catholic University of Leuven in Belgium and another of the paper’s senior authors, adapted a form of skull base surgery to remove tissue from the olfactory mucosa and bulb of Covid-19 patients within about an hour of their death. In 30 of the patients, the researchers were able to detect that the virus was still replicating – meaning the patients had died in the acute, contagious phase of the disease.
“It is unquestionably the most thoroughly done bit of work on human postmortem olfactory Covid tissue,” said Stuart Firestein, a neurobiologist at Columbia University in New York City.
But Firestein said the results did not shed much new light on how Covid-19 causes olfactory dysfunction. “They do not show any OSNs as being damaged or there being fewer of them, or the OSNs near infected sustentacular cells as being different in any way from those not near infected cells,” he said.
Debby Van Riel, a virologist at Erasmus University in Rotterdam, the Netherlands, also praised the study’s rigour, but said the authors’ claim that Sars-CoV-2 does not infect neurons was “pretty bold”.
In only six of the 30 patients was the virus detectable in the olfactory mucosa itself. “Overall the numbers are thus really low to make any strong conclusions,” she said.
But even if the study isn’t the last word on Covid’s brain effects, it does indicate that those dire early reports weren’t either. If its conclusions are borne out, those experiencing Covid-related anosmia or parosmia can be reassured that the virus has not infected their brains, and that future therapies targeting the understudied sustentacular cells could alleviate or cure their condition.
News
Most Plastic in the Ocean Is Invisible—And Deadly
Nanoplastics—particles smaller than a human hair—can pass through cell walls and enter the food web. New research suggest 27 million metric tons of nanoplastics are spread across just the top layer of the North [...]
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
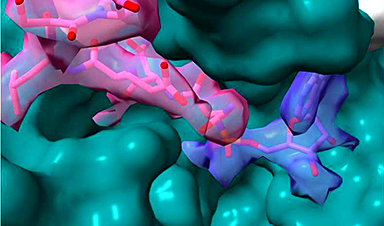
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
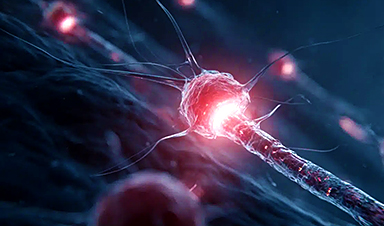
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
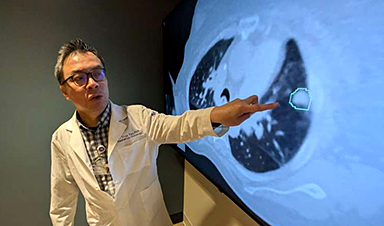
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]