Summary: A groundbreaking study reveals how obesity may drive Alzheimer’s disease through tiny messengers called extracellular vesicles released from fat tissue. These vesicles carry lipids that alter how quickly amyloid-β plaques form, a hallmark of Alzheimer’s.
Because they can cross the blood-brain barrier, they act as a direct communication line between body fat and the brain. Targeting these messengers could open new ways to prevent or slow dementia in at-risk individuals.
Key Facts:
- Fat-to-Brain Link: Extracellular vesicles from body fat can cross the blood-brain barrier.
- Plaque Formation: Vesicle lipids in obese individuals promote faster amyloid-β clumping.
- Therapeutic Potential: Blocking this signaling may reduce Alzheimer’s risk in obesity.
Source: Houston Methodist
Obesity has long been acknowledged as a risk factor for a wide range of diseases, but a more precise link between obesity and Alzheimer’s disease has remained a mystery – until now.
The study, “Decoding Adipose–Brain Crosstalk: Distinct Lipid Cargo in Human Adipose-Derived Extracellular Vesicles Modulates Amyloid Aggregation in Alzheimer’s Disease,” published today in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
It explores the link between obesity, which affects about 40% of the U.S population, and the dreaded neurodegenerative disease affecting more than 7 million people in the U.S.
The research was led by Stephen Wong, Ph.D., the John S. Dunn Presidential Distinguished Chair in Biomedical Engineering . Alongside Wong, Li Yang, Ph.D., a research associate at Houston Methodist, and Jianting Sheng, Ph.D., an assistant research professor of computational biology and mathematics in radiology at the Houston Methodist Academic Institute, provided leadership in experimental design and cross-institution coordination.
“As recent studies have underscored, obesity is now recognized as the top modifiable risk factor for dementia in the United States,” said Wong, corresponding author and director of T. T. & W. F. Chao Center for BRAIN at Houston Methodist.
The researchers found that the lipid cargo of these cell messengers differs between people with obesity and lean individuals, and that the presence and levels of specific lipids that differed between the groups changed how quickly amyloid-β clumped together in laboratory models.
Using mouse models and patient body fat samples, the researchers examined the vesicles, which are tiny, membrane-bound particles that travel throughout the body and act as messengers involved in cell-to-cell communication. These minuscule communicators are also capable of crossing the blood-brain barrier.
Targeting these tiny cell messengers and disrupting their communication that leads to plaque formation may help reduce the risk of Alzheimer’s disease in people with obesity. The researchers said future work should focus on how drug therapy could stop or slow the build-up of Alzheimer’s-related toxic proteins (such as amyloid-β) in at-risk individuals.
The research was coauthored by Michael Chan, Shaohua Qi, and Bill Chan from Houston Methodist; Dharti Shantaram, Xilal Rima, Eduardo Reategui, and Willa Hsueh from The Ohio State University’s Wexner Medical Center; and Xianlin Han from the University of Texas Health Science Center at San Antonio.
About this Alzheimer’s Disease research news
Author: Amy McCaig
Source: Houston Methodist
Contact: Amy McCaig – Houston Methodist
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Decoding Adipose–Brain Crosstalk: Distinct Lipid Cargo in Human Adipose-Derived Extracellular Vesicles Modulates Amyloid Aggregation in Alzheimer’s Disease” by Stephen Wong et al. Alzheimer’s & Dementia
Abstract
Decoding Adipose–Brain Crosstalk: Distinct Lipid Cargo in Human Adipose-Derived Extracellular Vesicles Modulates Amyloid Aggregation in Alzheimer’s Disease
INTRODUCTION
Obesity is a major modifiable risk factor for Alzheimer’s disease (AD), but the mechanistic link between peripheral metabolic dysfunction and AD progression remains unclear. Adipose-derived extracellular vesicles (EVs) may penetrate the brain and alter lipid homeostasis, contributing to neurodegeneration.
METHODS
We isolated exosome-enriched EVs from subcutaneous and visceral fat of lean and obese individuals, followed by lipidomic profiling. An in vitro amyloid-β (Aβ) aggregation assay using purified Aβ40 and Aβ42 peptides was performed under lipid environments mimicking physiological and pathological states.
RESULTS
Obese-derived EVs exhibited distinct lipid profiles, particularly in lysophosphatidylcholine (LPC) and sphingomyelin (SM) species. Functional assays demonstrated that lipid identity and concentration critically influenced Aβ aggregation kinetics.
DISCUSSION
Our study reveals that obesity-associated EV lipids modulate Aβ aggregation, linking adipose metabolism to AD pathology. These findings support lipid-targeted strategies as potential therapeutics for neurodegenerative diseases.
News
Scientists Crack a 50-Year Tissue Mystery With Major Cancer Implications
Researchers have resolved a 50-year-old scientific mystery by identifying the molecular mechanism that allows tissues to regenerate after severe damage. The discovery could help guide future treatments aimed at reducing the risk of cancer [...]
This New Blood Test Can Detect Cancer Before Tumors Appear
A new CRISPR-powered light sensor can detect the faintest whispers of cancer in a single drop of blood. Scientists have created an advanced light-based sensor capable of identifying extremely small amounts of cancer biomarkers [...]
Blindness Breakthrough? This Snail Regrows Eyes in 30 Days
A snail that regrows its eyes may hold the genetic clues to restoring human sight. Human eyes are intricate organs that cannot regrow once damaged. Surprisingly, they share key structural features with the eyes [...]
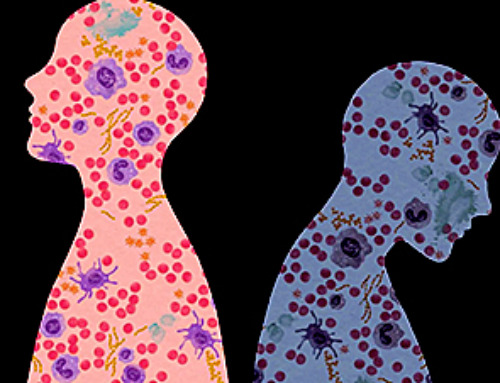
This Is Why the Same Virus Hits People So Differently
Scientists have mapped how genetics and life experiences leave lasting epigenetic marks on immune cells. The discovery helps explain why people respond so differently to the same infections and could lead to more personalized [...]
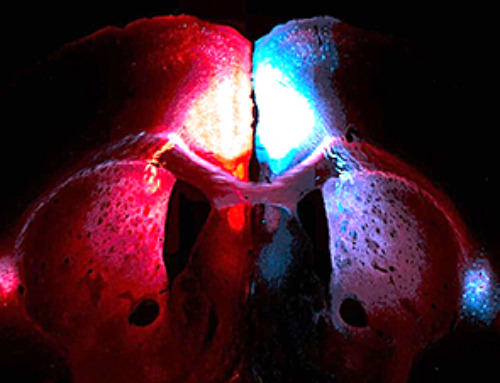
Rejuvenating neurons restores learning and memory in mice
EPFL scientists report that briefly switching on three “reprogramming” genes in a small set of memory-trace neurons restored memory in aged mice and in mouse models of Alzheimer’s disease to level of healthy young [...]
New book from Nanoappsmedical Inc. – Global Health Care Equivalency
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
New Molecule Blocks Deadliest Brain Cancer at Its Genetic Root
Researchers have identified a molecule that disrupts a critical gene in glioblastoma. Scientists at the UVA Comprehensive Cancer Center say they have found a small molecule that can shut down a gene tied to glioblastoma, a [...]
Scientists Finally Solve a 30-Year-Old Cancer Mystery Hidden in Rye Pollen
Nearly 30 years after rye pollen molecules were shown to slow tumor growth in animals, scientists have finally determined their exact three-dimensional structures. Nearly 30 years ago, researchers noticed something surprising in rye pollen: [...]
NanoMedical Brain/Cloud Interface – Explorations and Implications. A new book from Frank Boehm
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
How lipid nanoparticles carrying vaccines release their cargo
A study from FAU has shown that lipid nanoparticles restructure their membrane significantly after being absorbed into a cell and ending up in an acidic environment. Vaccines and other medicines are often packed in [...]
New book from NanoappsMedical Inc – Molecular Manufacturing: The Future of Nanomedicine
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
A Virus Designed in the Lab Could Help Defeat Antibiotic Resistance
Scientists can now design bacteria-killing viruses from DNA, opening a faster path to fighting superbugs. Bacteriophages have been used as treatments for bacterial infections for more than a century. Interest in these viruses is rising [...]
Sleep Deprivation Triggers a Strange Brain Cleanup
When you don’t sleep enough, your brain may clean itself at the exact moment you need it to think. Most people recognize the sensation. After a night of inadequate sleep, staying focused becomes harder [...]
Lab-grown corticospinal neurons offer new models for ALS and spinal injuries
Researchers have developed a way to grow a highly specialized subset of brain nerve cells that are involved in motor neuron disease and damaged in spinal injuries. Their study, published today in eLife as the final [...]
Urgent warning over deadly ‘brain swelling’ virus amid fears it could spread globally
Airports across Asia have been put on high alert after India confirmed two cases of the deadly Nipah virus in the state of West Bengal over the past month. Thailand, Nepal and Vietnam are among the [...]
This Vaccine Stops Bird Flu Before It Reaches the Lungs
A new nasal spray vaccine could stop bird flu at the door — blocking infection, reducing spread, and helping head off the next pandemic. Since first appearing in the United States in 2014, H5N1 [...]