In efforts to tackle the leading cause of blindness in developed countries, researchers have recruited nanotechnology to help regrow retinal cells.
Macular degeneration is a form of central vision loss, which has massive social, mobility, and mental consequences. It impacts hundreds of millions of people globally and is increasing in prevalence.
The degeneration is the consequence of damaged retinal pigment cells. Our bodies are unable to grow and replace these cells once they start dying, so scientists have been exploring alternative methods to replace them and the membrane within which they sit.
“In the past, scientists would grow cells on a flat surface, which is not biologically relevant,” explains Anglia Ruskin University biochemist Barbara Pierscionek.
“Using these new techniques the cell line has been shown to thrive in the 3D environment provided by the scaffolds.”
Nottingham Trent University biomedical scientist Biola Egbowon and colleagues fabricated these 3D scaffolds with polymer nanofibers and coated them with a steroid to reduce inflammation.
Using a technique called electrospinning, which produces nanometer-wide fibers by squirting a molten polymer through a high-voltage field, the team was able to keep the scaffold sufficiently thin.
The polyacrylonitrile polymer they used provided mechanical strength, and Jeffamine polymer attracts water, essentially allowing the synthetic scaffold to act as a membrane.
The water-attracting ability of the material is what helps the cells bind to the scaffold and also encourages their growth, but when the effect is too strong, it’s also been associated with cell death in previous research.
The team’s new formulation seems to be just right, as the system increased the growth and longevity of the retinal lab cells and kept them viable for at least 150 days.
“This research has demonstrated, for the first time, that nanofiber scaffolds treated with the anti-inflammatory substance such as fluocinolone acetonide can enhance the growth, differentiation, and functionality of retinal pigment epithelial cells,” says Pierscionek.
Previous attempts have used collagen and cellulose to create a similar scaffold, but Egbowon and team believes their synthetic option will be easier to make compatible with our immune systems and simpler to modify.
The new study has demonstrated this method can keep the required single layer of retinal cells healthy, producing biomarkers that indicate they are functioning more naturally than what has been found when they grow on other mediums.
However, there’s still a lot we don’t know about how viable this approach will be for treating human patients with macular degeneration.
“While this may indicate the potential of such cellularized scaffolds in regenerative medicine, it does not address the question of biocompatibility with human tissue,” Egbowon and colleagues caution in their paper, as there is a massive difference between growing cells in a petri dish and having a functioning tissue substitute within a body.
Other research in this area is already investigating whether lab grown cells can be plugged back into other retinal cell types to form functioning units of tissue. Another tactic involves activating cells already in human eye tissues that regenerate retinal cells in other animals.
The team’s next steps will be to investigate the orientation of the cells, which is important for ensuring they can maintain a good blood supply, before they can be considered for testing inside a living system.
This research was published in Materials & Design.
News
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
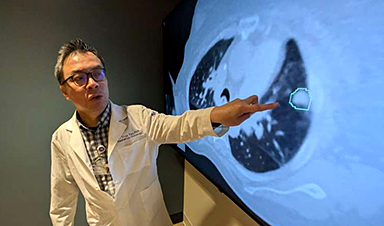
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]