The new test could help identify which patients are most likely to benefit from new Alzheimer's drugs.
A newly developed blood test for Alzheimer's disease not only helps confirm the presence of the condition but also provides information about how far the disease has progressed, according to research from Washington University School of Medicine in St. Louis and Lund University in Sweden.
While several Alzheimer's blood tests are already available, including two based on technology licensed from Washington University, those existing tests mainly assist in diagnosing the disease in people showing cognitive symptoms. However, they do not reveal how advanced the symptoms are or the extent of cognitive decline caused by Alzheimer's dementia. This distinction is important because current treatments for Alzheimer's are most effective in the early stages. A reliable, accessible method to assess disease progression could help doctors identify which patients are most likely to benefit from treatment and how aggressively they should be treated.
The new test also offers valuable insight into whether a person's symptoms are due to Alzheimer's or another underlying condition.
The study was recently published in the journal Nature Medicine.
In the study, the researchers found that levels of a protein called MTBR-tau243 in the blood accurately reflect the amount of toxic accumulation of tau aggregates in the brain and correlate with the severity of Alzheimer's disease. Analyzing blood levels of MTBR-tau243 from a group of people with cognitive decline, the researchers were able to distinguish between people with early- or later-stage Alzheimer's disease and separate both groups of Alzheimer's patients from people whose symptoms were caused by something other than Alzheimer's disease.
"This blood test clearly identifies Alzheimer's tau tangles, which is our best biomarker measure of Alzheimer's symptoms and dementia," said co-senior author Randall J. Bateman, MD, the Charles F. and Joanne Knight Distinguished Professor of Neurology at WashU Medicine. "In clinical practice right now, we don't have easy or accessible measures of Alzheimer's tangles and dementia, and so a tangle blood test like this can provide a much better indication if the symptoms are due to Alzheimer's and may also help doctors decide which treatments are best for their patients."
Tracking Alzheimer's disease progression from blood
Alzheimer's disease involves a build-up of a protein, called amyloid, into plaques in the brain, followed by the development of tangles of tau protein years later. Cognitive symptoms emerge around the time tau tangles become detectable, and symptoms worsen as the tangles spread. The gold standard for staging Alzheimer's disease is positron emission tomography (PET) brain scans for amyloid plaques and tau tangles. Amyloid scans yield information about the presymptomatic and early symptomatic stages, while tau scans are useful for tracking later stages of the disease. PET brain scans are highly accurate but expensive, time-consuming, and frequently unavailable outside of major research centers, so they are not widely used.
Bateman leads a team that is developing blood tests for Alzheimer's disease as a more accessible alternative to brain scans. They have developed two blood tests that correlate closely with the amount of amyloid plaques in the brain. Both are now used by doctors to aid diagnosis. But until now, there has been no blood test that reports on tau levels in the brain.
In a previous study, Bateman and colleagues — including co-first authors Kanta Horie, PhD, a research associate professor of neurology at WashU Medicine, and Gemma Salvadó, PhD, then a postdoctoral researcher at Lund University, and co-senior author Oskar Hansson, MD, PhD, a professor of neurology at Lund University — showed that cerebrospinal fluid levels of MTBR-tau243 correlate closely with tau tangles in the brain. In the current study, the team extended the analysis to blood. A blood sample is easier to collect than cerebrospinal fluid, which is obtained via spinal tap.

The researchers developed a technique to measure MTBR-tau243 levels in people's blood and compared it to the amount of tau tangles in their brains as measured by brain scans. They piloted the approach on data from two cohorts: volunteers at WashU Medicine's Charles F. and Joanne Knight Alzheimer Disease Research Center, which included 108 people, and a subset of 55 people from the Swedish BioFINDER-2 cohort. To assess whether the approach was generalizable, they validated it in an independent dataset consisting of the remaining 739 people in the BioFINDER-2 cohort.
The people in the two cohorts represented all but the most severe end of the spectrum of Alzheimer's disease, from the presymptomatic stage when brain amyloid levels are elevated but people remain cognitively healthy, through early-stage disease with mild cognitive impairments, to late symptomatic disease when patients exhibit full-blown dementia. For comparison, cognitively healthy people with normal amyloid levels, and people with cognitive symptoms due to conditions other than Alzheimer's disease, were included.
The researchers' analysis showed that blood MTBR-tau243 levels reflected the amount of tau tangles in the brain with 92% accuracy. MTBR-tau243 levels in the blood were normal in asymptomatic people regardless of amyloid status, meaning that blood MTBR-tau243 levels do not change between healthy people and people in the presymptomatic stage of Alzheimer's disease with amyloid plaques.
Among people with cognitive symptoms due to Alzheimer's disease, MTBR-tau243 levels were significantly elevated for people in the mild cognitive impairment phase of Alzheimer's disease and much higher — up to 200 times — for those in the dementia phase. Those differences translated into clear separation of people in early- and late-stage Alzheimer's disease. At the same time, MTBR-tau243 levels were normal in people with cognitive symptoms due to diseases other than Alzheimer's, meaning that the test effectively distinguished Alzheimer's dementia from other kinds of dementia.
The technology underlying the blood test for tau aggregates has been licensed by WashU to C2N Diagnostics, a WashU startup that developed the blood tests for amyloid. These amyloid tests incorporate measures of another form of tau called p-tau217.
"I believe we will use blood-based p-tau217 to determine whether an individual has Alzheimer's disease, but MTBR-tau243 will be a highly valuable complement in both clinical settings and research trials," said Hansson. "When both of these biomarkers are positive, the likelihood that Alzheimer's is the underlying cause of a person's cognitive symptoms increases significantly, compared to when only p-tau217 is abnormal. This distinction is crucial for selecting the most appropriate treatment for each patient."
Blood tests could inform personalized Alzheimer's treatment
Two Alzheimer's therapies have been approved by the Food and Drug Administration (FDA) to slow progression of the disease, and both work by lowering amyloid levels in the brain. Horie said the number and variety of available Alzheimer's medications may soon be expanding, as several experimental drugs that target tau or other aspects of Alzheimer's disease are in the pipeline. With blood tests to diagnose and stage the disease, doctors would be able to tailor treatments to the patient's particular disease state.
"We're about to enter the era of personalized medicine for Alzheimer's disease," Horie said. "For early stages with low tau tangles, anti-amyloid therapies could be more efficacious than in late stages. But after the onset of dementia with high tau tangles, anti-tau therapy or one of the many other experimental approaches may be more effective. Once we have a clinically available blood test for staging, plus treatments that work at different stages of the disease, doctors will be able to optimize their treatment plans for the specific needs of each patient."
Reference: "Plasma MTBR-tau243 biomarker identifies tau tangle pathology in Alzheimer's disease" by Kanta Horie, Gemma Salvadó, Rama K. Koppisetti, Shorena Janelidze, Nicolas R. Barthélemy, Yingxin He, Chihiro Sato, Brian A. Gordon, Hong Jiang, Tammie L. S. Benzinger, Erik Stomrud, David M. Holtzman, Niklas Mattsson-Carlgren, John C. Morris, Sebastian Palmqvist, Rik Ossenkoppele, Suzanne E. Schindler, Oskar Hansson and Randall J. Bateman, 31 March 2025, Nature Medicine.
DOI: 10.1038/s41591-025-03617-7
This work was supported by the Charles F. and Joanne Knight Alzheimer Disease Research Center; the Tracy Family SILQ Center; the National Institutes of Health (NIH), grant number R01AG070941; the Alzheimer's Association's Zenith Award; the Hope Center for Neurological Disorders; and the Department of Neurology at WashU Medicine. The Swedish BioFINDER-2 study was supported by the U.S. National Institute on Aging, grant number R01AG083740, the European Research Council, grant number ADG-101096455; the Alzheimer's Association, grant numbers ZEN24-1069572 and SG-23-1061717; the GHR Foundation; the Swedish Research Council, grant numbers 2022-00775, 2021-02219, and 2018-02052; ERA PerMed, grant number ERAPERMED2021-184; the Knut and Alice Wallenberg foundation, grant number 2022-0231; the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson's disease) at Lund University; the Swedish Alzheimer Foundation, grant numbers AF-980907, AF-994229, and AF-994075; the Swedish Brain Foundation, grant numbers FO2021-0293, FO2023-0163 and FO2022-0204; the Wallenberg AI, Autonomous Systems and Software Program (WASP) and the SciLifeLab and Wallenberg National Program for Data-Driven Life Science (DDLS) joint call for research projects, grant number WASP/DDLS22-066; the Parkinson foundation of Sweden, grant number 1412/22; the Cure Alzheimer's fund; the Rönström Family Foundation; the Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse; the Skåne University Hospital Foundation, grant number 2020-O000028; the Regionalt Forskningsstöd, grant number 2022-1259; and the Swedish federal government under the ALF agreement, grant numbers 2022-Projekt0080 and 2022-Projekt0107. Gemma Salvadó received funding from the European Union's Horizon 2020 Research and Innovation Program under Marie Sklodowska-Curie action grant agreement number 101061836; the Alzheimer's Association, fellowship number AARF-22-972612; the Alzheimerfonden, grant number AF-980942; BrightFocus Foundation, fellowship number A2024007F; Greta och Johan Kocks; and the Strategic Research Area MultiPark (Multidisciplinary Research in Parkinson's Disease) at Lund University.
News
This Simple Brain Exercise May Protect Against Dementia for 20 Years
A long-running study following thousands of older adults suggests that a relatively brief period of targeted brain training may have effects that last decades. Starting in the late 1990s, close to 3,000 older adults [...]
Scientists Crack a 50-Year Tissue Mystery With Major Cancer Implications
Researchers have resolved a 50-year-old scientific mystery by identifying the molecular mechanism that allows tissues to regenerate after severe damage. The discovery could help guide future treatments aimed at reducing the risk of cancer [...]
This New Blood Test Can Detect Cancer Before Tumors Appear
A new CRISPR-powered light sensor can detect the faintest whispers of cancer in a single drop of blood. Scientists have created an advanced light-based sensor capable of identifying extremely small amounts of cancer biomarkers [...]
Blindness Breakthrough? This Snail Regrows Eyes in 30 Days
A snail that regrows its eyes may hold the genetic clues to restoring human sight. Human eyes are intricate organs that cannot regrow once damaged. Surprisingly, they share key structural features with the eyes [...]
This Is Why the Same Virus Hits People So Differently
Scientists have mapped how genetics and life experiences leave lasting epigenetic marks on immune cells. The discovery helps explain why people respond so differently to the same infections and could lead to more personalized [...]
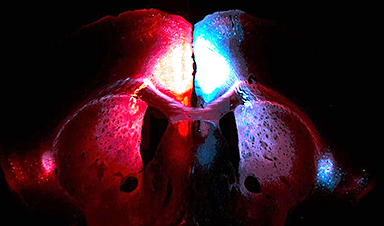
Rejuvenating neurons restores learning and memory in mice
EPFL scientists report that briefly switching on three “reprogramming” genes in a small set of memory-trace neurons restored memory in aged mice and in mouse models of Alzheimer’s disease to level of healthy young [...]
New book from Nanoappsmedical Inc. – Global Health Care Equivalency
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
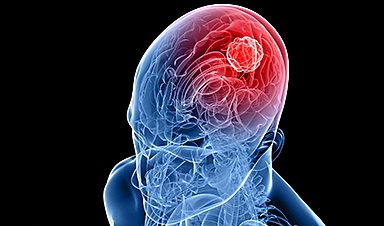
New Molecule Blocks Deadliest Brain Cancer at Its Genetic Root
Researchers have identified a molecule that disrupts a critical gene in glioblastoma. Scientists at the UVA Comprehensive Cancer Center say they have found a small molecule that can shut down a gene tied to glioblastoma, a [...]
Scientists Finally Solve a 30-Year-Old Cancer Mystery Hidden in Rye Pollen
Nearly 30 years after rye pollen molecules were shown to slow tumor growth in animals, scientists have finally determined their exact three-dimensional structures. Nearly 30 years ago, researchers noticed something surprising in rye pollen: [...]
NanoMedical Brain/Cloud Interface – Explorations and Implications. A new book from Frank Boehm
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
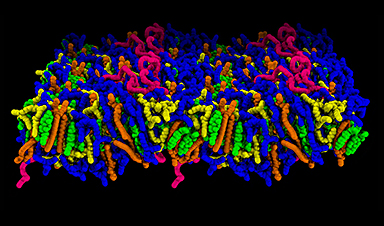
How lipid nanoparticles carrying vaccines release their cargo
A study from FAU has shown that lipid nanoparticles restructure their membrane significantly after being absorbed into a cell and ending up in an acidic environment. Vaccines and other medicines are often packed in [...]
New book from NanoappsMedical Inc – Molecular Manufacturing: The Future of Nanomedicine
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
A Virus Designed in the Lab Could Help Defeat Antibiotic Resistance
Scientists can now design bacteria-killing viruses from DNA, opening a faster path to fighting superbugs. Bacteriophages have been used as treatments for bacterial infections for more than a century. Interest in these viruses is rising [...]
Sleep Deprivation Triggers a Strange Brain Cleanup
When you don’t sleep enough, your brain may clean itself at the exact moment you need it to think. Most people recognize the sensation. After a night of inadequate sleep, staying focused becomes harder [...]
Lab-grown corticospinal neurons offer new models for ALS and spinal injuries
Researchers have developed a way to grow a highly specialized subset of brain nerve cells that are involved in motor neuron disease and damaged in spinal injuries. Their study, published today in eLife as the final [...]
Urgent warning over deadly ‘brain swelling’ virus amid fears it could spread globally
Airports across Asia have been put on high alert after India confirmed two cases of the deadly Nipah virus in the state of West Bengal over the past month. Thailand, Nepal and Vietnam are among the [...]