AZoNano speak to Dr. Dominik Rejman about the innovative wound treatment, NANO-LLPO. This nanofibrous dressing can not only help to prevent bacterial infection but can promote wound healing as well. Read more about the research behind this exciting development, and how it is helping to advance the integration of nanotechnology in biomedicine.
Please could you introduce yourself and tell us what inspired your career in biotechnology research?
My name is Dominik Rejman, and I am a group leader at the Institute of Organic Chemistry and Biochemistry of the Czech Academy of Sciences, Prague (IOCB Prague). I graduated from the UTC Prague from organic chemistry and continued towards Ph.D. study at the IOCB Prague in the field of modified nucleosides, nucleotides, and oligonucleotides.
Since these molecules often possess fascinating biological properties, I have been connected with biochemistry, biology, and medicinal chemistry from the very beginning of my carrier. During my first postdoc position at the University of Sheffield, I worked on dinucleoside polyphosphates and their analogs. Then, I dealt with inhibitors of IMPDH and antiparasitic compounds in the Center for Drug Design at the University of Minnesota.
When I returned to Prague, my focus was aimed at antimicrobial compounds and, in general, new strategies to understand and treat infectious diseases.
How did you begin your involvement with nanomaterials?
Capitalizing on my antiparasitic compounds research, I have discovered, in collaboration with L. Krásný from the Institute of Microbiology and M. Kolář from the Palacký University Olomouc, novel antimicrobial compounds termed lipophosphonoxins (LPPO).
Following a lecture I gave on this subject, I was approached by the Head of Prague Burn Center R. Zajíček. He expressed his concern about infections in burn patients, and since he was involved in clinical trials of new nanomaterial fiber dressing NANOTARDIS developed in the Technical University, Liberec (TUL), we ended up with the idea of combining our molecules with the new nanomaterial.
Could you give an overview of your research?
I collaborated with professor D. Lukáš from TUL on this new composite material. First, we developed the fabrication method and then evaluated its antibacterial and mechanical properties. Finally, we performed the first in vivo experiment to validate its use in infectious wounds, which was quite successful.
NANO-LPPO is an exciting innovation in preventing skin infections as well as preventing bacterial strain resistance. Could you explain how this development compares to existing treatment methods?
The nanomaterial itself can promote wound healing, forming a sort of scaffold for cells to grow. An important property is also its biodegradability, mediated by enzymes lipases that are present in the wound.
When we combine the nanomaterial with our antibacterial LPPO, the LPPO is released mostly via biodegradation.
The presence of LPPO in the material increases the rate of degradation. This technology is particularly interesting because bacteria in the wound excrete the lytic enzymes and thus enhance biodegradation, releasing the antibacterial component LPPO.
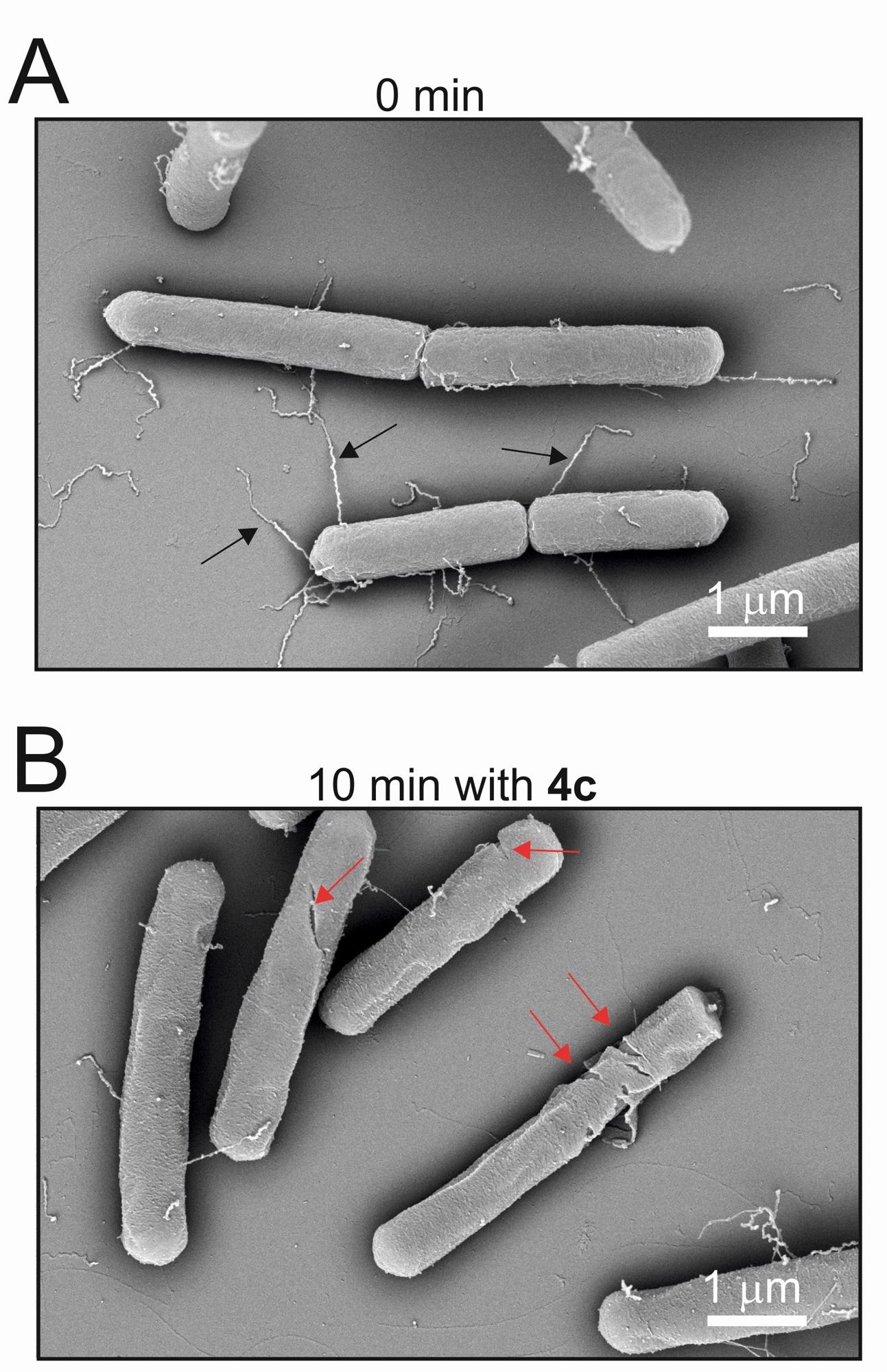
Bacillus subtilis bacteria before and after application of LPPO. The second image shows significant damage to bacteria after ten minutes. Image Credit: Institute of Microbiology of the CAS
In other words, the release of the antibacterial compound is partly controlled by the presence of the bacteria. Another important property is that the antibacterial component exerts its activity only at the site of infection. As it is not absorbed, it should not, in principle, form selection pressure for resistance development.
Moreover, we know it is very difficult for bacteria to develop resistance against LPPO – so far, we have been unable to select a resistant strain against LPPO, which is fantastic.
The effect of different concentrations of LPPO was tested on the nanofibrous wound dressings. How might different LPPO concentrations affect the ability of the nanofiber as a wound dressing?
The optimal LPPO concentration for the NANO-LPPO composite material needs to be addressed in the next experiments. So far, 5-10% seems to be sufficient to prevent infection in the wound, at least for S. aureus.
A key aspect of the methodology was defining the wettability of the wound dressing. What other parameters are important to address when designing active, biocompatible nanomaterials?
The wettability measurement was key to understanding why the presence of LPPO in the NANO-LPPO enhances its biodegradability. Other important parameters include the rate of degradation and the rate of LPPO release to the wound.
Another is the hydrophobicity of the material, which can be modified by the presence of the LPPO, as we showed, or by alteration of the polymeric composition of the nanomaterial itself.
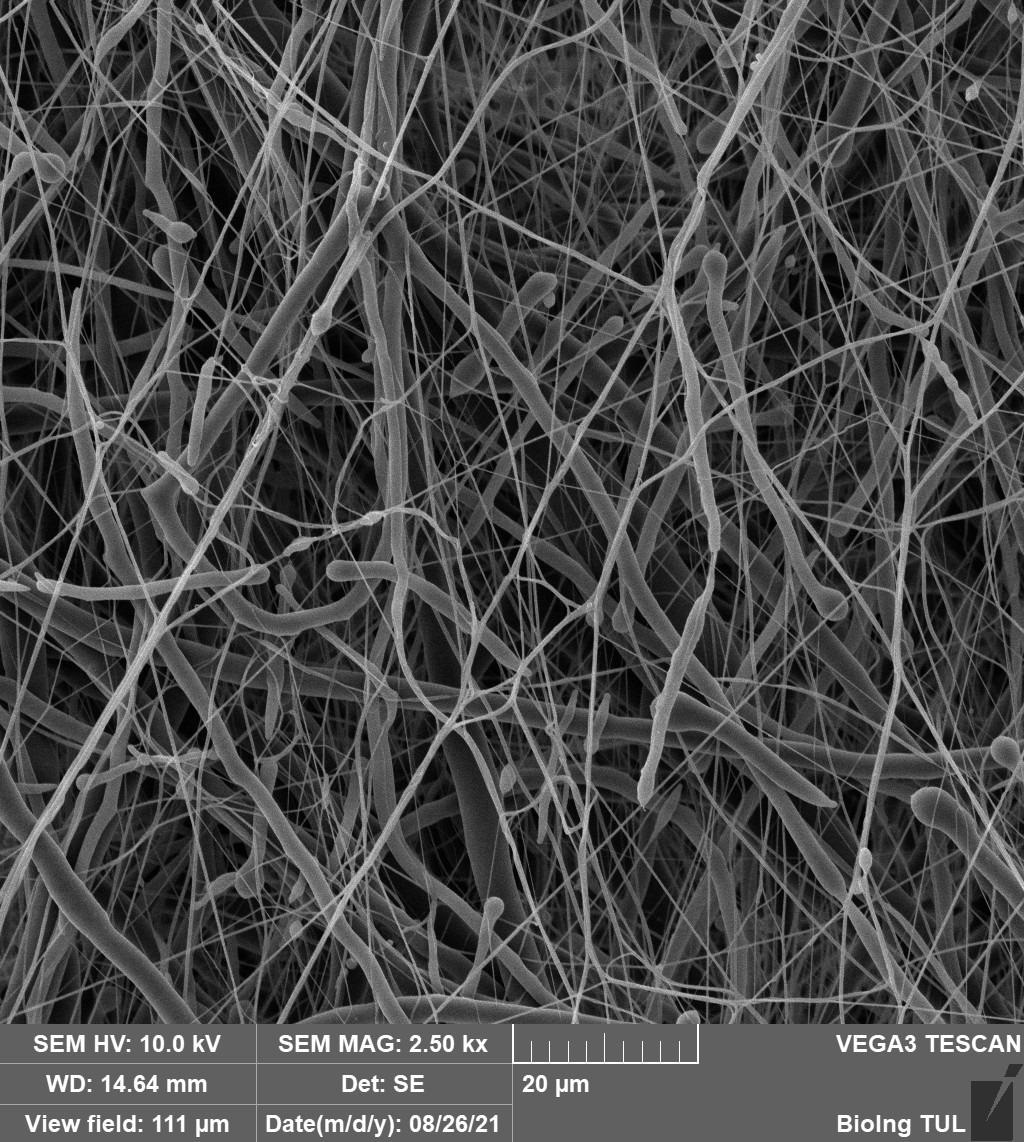
Nonwoven nanotextile NANOTARDIS. With its morphological and physical-chemical properties, the device promotes the healing of clean acute wounds. Image Credit: Technical University of Liberec
What major obstacles do you believe currently limit the involvement of nanofibers, and more broadly nanomaterials, for clinical applications?
I do not see any serious obstacle limiting the use of nanofibers. I see some concerns regarding the use of some nanoparticles due to their accumulation in tissues and potential chronic toxicity.
Infection treatment and promoting tissue regeneration are also important for internal damage. How could this research be extended to this application?
For internal use, where we can expect more systemic exposure to the antibacterial component, an antibacterial compound with extremely low systemic toxicity and minimal tendency to select for resistance is necessary. We hope this may be the next generation of LPPO, which we are currently working on.
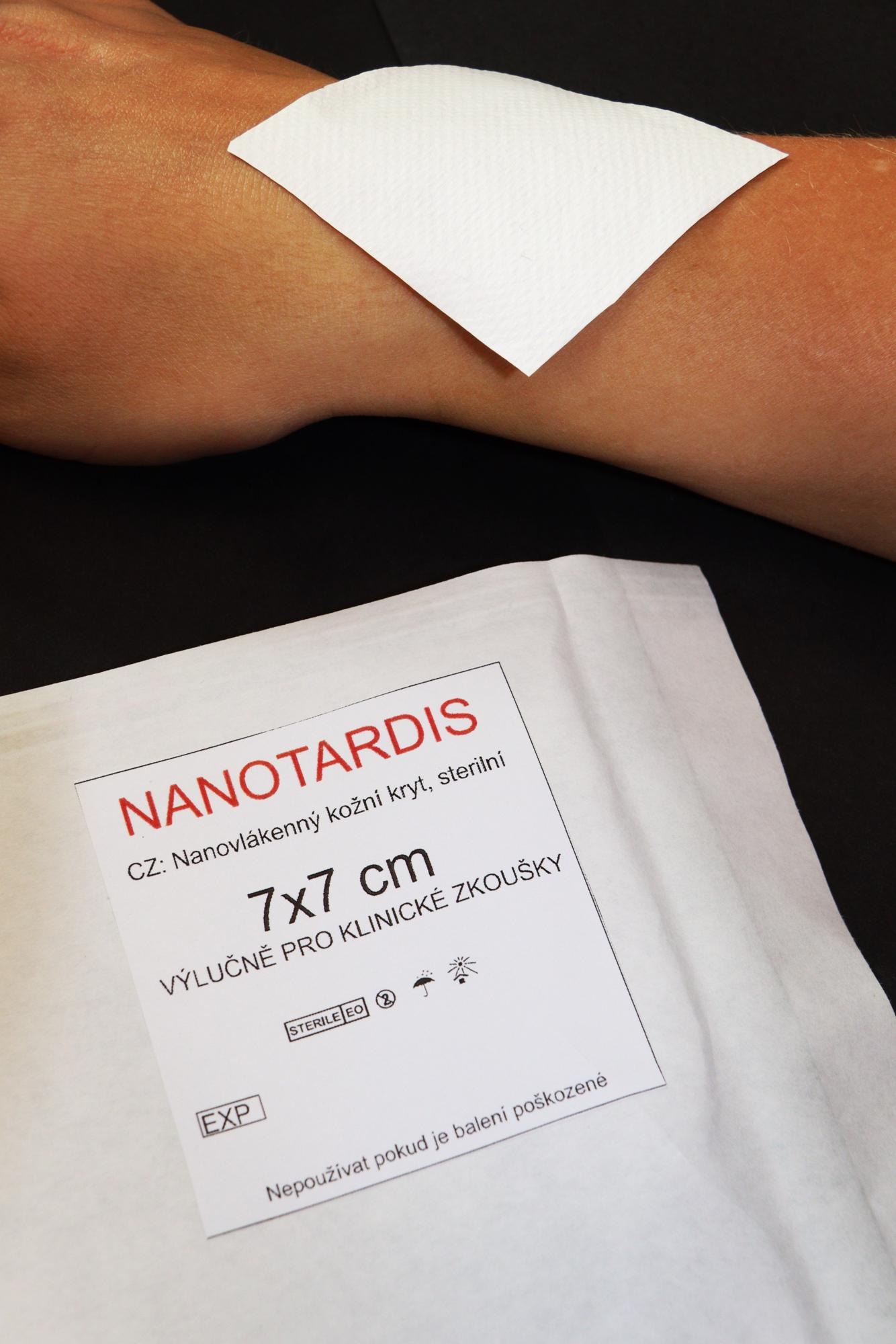
Nonwoven nanotextile NANOTARDIS. With its morphological and physical-chemical properties, the device promotes the healing of clean acute wounds. Image Credit: Technical University of Liberec
What are the next steps for this research, and more broadly the role of nanofibers and nanomaterials in clinical applications?
The next step in the research of NANO-LPPO will be the next phase of preclinical evaluation. This will involve a pig model, which is more relevant in terms of wound healing. When successful, then clinical evaluation can start.
I am optimistic about the use of modified nanofibrous materials in clinics, so I believe in 20 years, they will be a common tool in hospitals. I also expect that nanomaterial-based dressings for personal use will become commercially available.
News
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
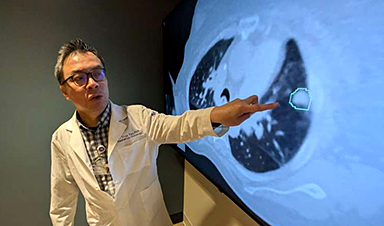
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]