More profoundly than previously believed, the virus that causes COVID-19, SARS-CoV-2, can impact the brain for months after infection. The findings were presented at Neuroscience 2022, the annual meeting of the Society for Neuroscience and the world’s largest source of emerging news about brain science and health.
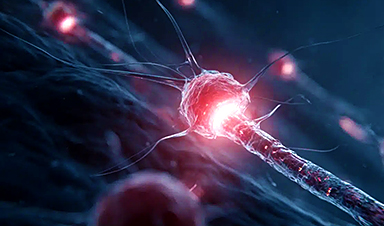
“Long COVID,” which includes the neurological fallout (a.k.a. sequelae) of a COVID-19 infection, can damage the central nervous system long after the acute symptoms of the virus have passed. Estimates report that one in five to one half of all adults are affected by at least one long COVID symptom, which includes ailments to mood and concentration. Scientists are still learning how the virus changes the brain, but it’s becoming increasingly clear that the long-term effects are wide-ranging across age groups.
Today’s new findings show that:
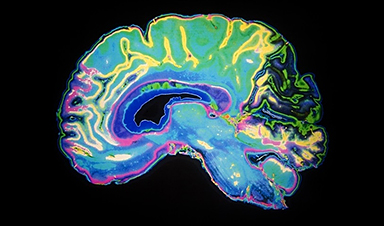
- Using fMRI imaging, scientists found that the sensorimotor brain regions of children who contracted COVID-19 months ago now showed a higher demand for resources. (Silvia Hidalgo-Tobon, UAM-Hospital Infantil de Mexico Federico Gomez)
- To mimic SARS-CoV-2’s impacts, scientists triggered inflammation in a mouse model via toll-like receptor (TLR) 7. Eight weeks later, they found hippocampal impairment in both sexes and decreased fear conditioning in males. (Natalie C. Tronson, University of Michigan)
- Scientists found that roughly one-fourth of adults who had mild COVID-19 four months prior were left with deficits in their visuoconstructive abilities. (Marco Aurelio Romano-Silva, Universidade Federal De Minas Gerais)
This isn’t the first time that a flu-like viral infection has been linked to an increased risk for dementia. But one of the most important aspects of this work is the magnitude of people potentially affected by this -; millions upon millions.”
Robyn Klein, The Robert E. and Louise F. Dunn Distinguished Professor of Medical Sciences, director of the Center for Neuroimmunology & Neuroinfectious Diseases, professor of medicine, pathology & immunology, and neurosciences at Washington University School of Medicine, and moderator
“We need to move on to alternative hypotheses for these neurologic diseases; we also need to inform the public and physicians that this is a real illness and that they should be proactive in addressing it.”
This research was supported by national funding agencies including the National Institutes of Health and private funding organizations. Find out more about COVID-19 and cognitive functioning on BrainFacts.org.
News
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
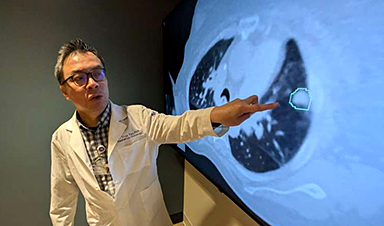
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]