“It is a very serious disease with serious complications from which patients die relatively young,” says hematologist Linet Njue, senior physician at Inselspital Bern. According to the doctor, around 100 patients with the disease are being treated in large university hospitals in Switzerland, but the exact number is not recorded. It is one of the most common hereditary diseases worldwide.
The disease is caused by a gene that carries the blueprint for the red blood pigment haemoglobin. A gene mutation crystallizes the hemoglobin, causing the normally round red blood cells to deform into sickles. These, in turn, clog the bloodstream.
Now, the UK Medicines Agency has given the green light for a new gene therapy for sickle cell anaemia patients aged 12 and over. It is called Exacel (brand name “Casgevy”) and was developed by the companies Vertex Pharmaceuticals and CRISPR Therapeutics, the latter based in Zug.
It is the first ever approved treatment based on the CRISPR/Cas9 gene scissors. This is the technology that can precisely cut through and modify the genetic material and for the discovery of which the Nobel Prize in Chemistry was awarded in 2020.
No need for a foreign donor anymore
Victoria Gray, now 37, was the first person to be treated with the therapy in 2019. Thanks to the new “supercells”, her life has changed completely, she recently said. She now lives free of pain, can go back to work and take care of her four children.
Exacel has now been tested on around forty sickle cell anemia patients. As Vertex Pharmaceuticals and CRISPR Therapeutics have announced, additional clinical trials with children between the ages of 2 and 11 are now to begin. An application for approval for the therapy has not yet been received from the companies in Switzerland, as Swissmedic confirmed on request.
How Exacel Therapy WorksExacel does not target the disease-causing and mutated HBB gene, which causes the sickle-shaped blood cells. Rather, the therapy is dedicated to the gene called BCL11A. This gene is activated at birth and thus inhibits the formation of haemoglobin, which is actually only produced in the fetus. Exacel then cuts BCL11A apart, which deactivates the gene again and resumes prenatal hemoglobin production. This provides additional hemoglobin that is not malformed. The symptoms of the disease disappear. (sny)
Jacob Corn is Professor of Genome Biology at ETH Zurich and has been working on CRISPR treatments for years, including for sickle cell disease. “The whole CRISPR community is in a frenzy. The Exacel successes are impressive,” he says.
Nevertheless, it is crucial to accompany the treated patients over a long period of time, the regulatory authorities require at least 15 years. This is the only way to rule out long-term side effects, such as an increased risk of blood cancer – a concern that worries some scientists. However, Corn emphasizes: “At the moment, things are looking really good.”
According to the ETH professor, the CRISPR gene scissors offer a gateway to a new world of medicine. He draws a comparison:
It’s the same with hereditary diseases so far: You can make a genetic diagnosis to suffering patients, but you can’t offer them a therapy – that’s changing now.
There are more than 7000,1 diseases that are based on a single gene mutation, such as sickle cell anemia, and dozens of therapies are already in the pipeline, for example against the metabolic disease called familial hypercholesterolemia, which affects about 200 in <> people in Switzerland.
Due to the disease, a dangerous amount of cholesterol always remains in the blood. This greatly increases the risk of a heart attack or stroke. Studies with the CRISPR therapy from the biotech company Verve Therapeutics have so far been promising, even suggesting that “the world’s biggest killer” can soon be stopped, according to the headline of the US magazine “MIT Technology Review”.
Targeting multiple genes is much more difficult
Other diseases in the focus of the genetic engineers are cystic fibrosis, Duchenne muscular dystrophy or progeria, in which affected children age as if in fast motion. In addition to these single-mutation diseases, there are countless other diseases that are based on a combination of several gene mutations and environmental factors: Alzheimer’s, arthritis, many cancers, diabetes, autism spectrum disorders are just a few examples.
Another hurdle of future CRISPR therapies is those diseases that affect organs that are difficult to reach. In sickle cell anemia, it is comparatively easy to extract the blood cells from the body, manipulate them and return them. “In cystic fibrosis, on the other hand, where the lungs are damaged, it is a much more difficult procedure to get the genetic medicine to the right place,” says Corn.
The high cost could limit availability
Geneticists are very worried about the horrendous costs, which are estimated to run into the millions for a single CRISPR treatment. It is questionable whether poorer countries can afford such therapies. Even rich countries get into trouble when a large number of patients suddenly want to be treated.
One dilemma, according to Jacob Corn, is that the safety requirements imposed by the health authorities are enormously high – and therefore costly. “That’s good, because it must be guaranteed that the therapies do no more harm than good.” The hope is that after the first approvals, the multitude of safety and efficacy tests will no longer have to be carried out every single time. “If the safety of CRISPR technology is proven on its own, then hopefully it would be legitimate to accelerate the testing and approval of therapies for other diseases,” says Corn.
Another approach: Instead of isolating the cells for the gene changes, treating them and then injecting them back into the body, researchers are tinkering with a gene injection: “The idea is that the genome editing process is injected into the body, so to speak, where it finds the right place and exerts its effect.” This would not only make treatment cheaper, but also more accessible, for example in regions of Africa where there are few health facilities. No tests have yet been carried out in humans, only in animals.
But Jacob Corn is confident: “A large number of research groups around the world are involved in CRISPR. How quickly things can sometimes happen when many bright minds are working on a problem at the same time was seen with the Corona vaccination.” (aargauerzeitung.ch)
News
Repurposed drugs could calm the immune system’s response to nanomedicine
An international study led by researchers at the University of Colorado Anschutz Medical Campus has identified a promising strategy to enhance the safety of nanomedicines, advanced therapies often used in cancer and vaccine treatments, [...]
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
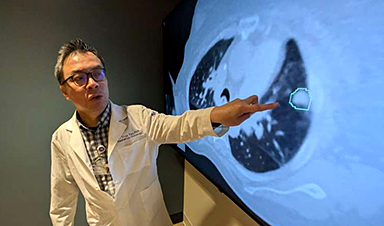
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]