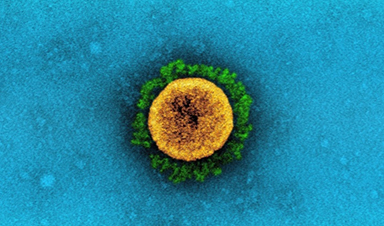
A study conducted at the New York City Department of Health and Mental Hygiene, USA, and the Mailman School of Public Health, Columbia University, USA, has determined the transmission rate, immune escape ability, and infection fatality rate of the B.1.526 variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The findings reveal that the variant has considerably higher transmissibility and immune escape potential than previously circulating variants and that it can increase the infection fatality rate by 62% – 82% among older adults. The study is currently available on the medRxiv* preprint server.
Background
With the progression of the coronavirus disease 2019 (COVID-19) pandemic, several new variants of SARS-CoV-2 have been identified. Because of increased infectivity and pathogenicity, some of these variants have been designated as Variants of Concern (VOC) or Variants of Interest (VOI) by the World Health Organization (WHO).
The B.1.526 variant of SARS-CoV-2, also known as the lota variant, was first identified in New York City in November 2020. Later, the variant has been detected in all 52 states in the United States, as well as in 27 countries across the world.
As observed in a laboratory-based study, this variant is modestly resistant to neutralization by therapeutic monoclonal antibodies and vaccine/infection-induced antibodies. In contrast, evidence indicates that the variant does not increase the risk of breakthrough infections in vaccinated or previously infected individuals.
In the current study, the scientists have analyzed multiple epidemiological and population datasets collected in New York City and performed mathematical modeling to determine the transmission rate, immune evasion ability, and infection fatality risk of the B.1.526 variant.
Study design
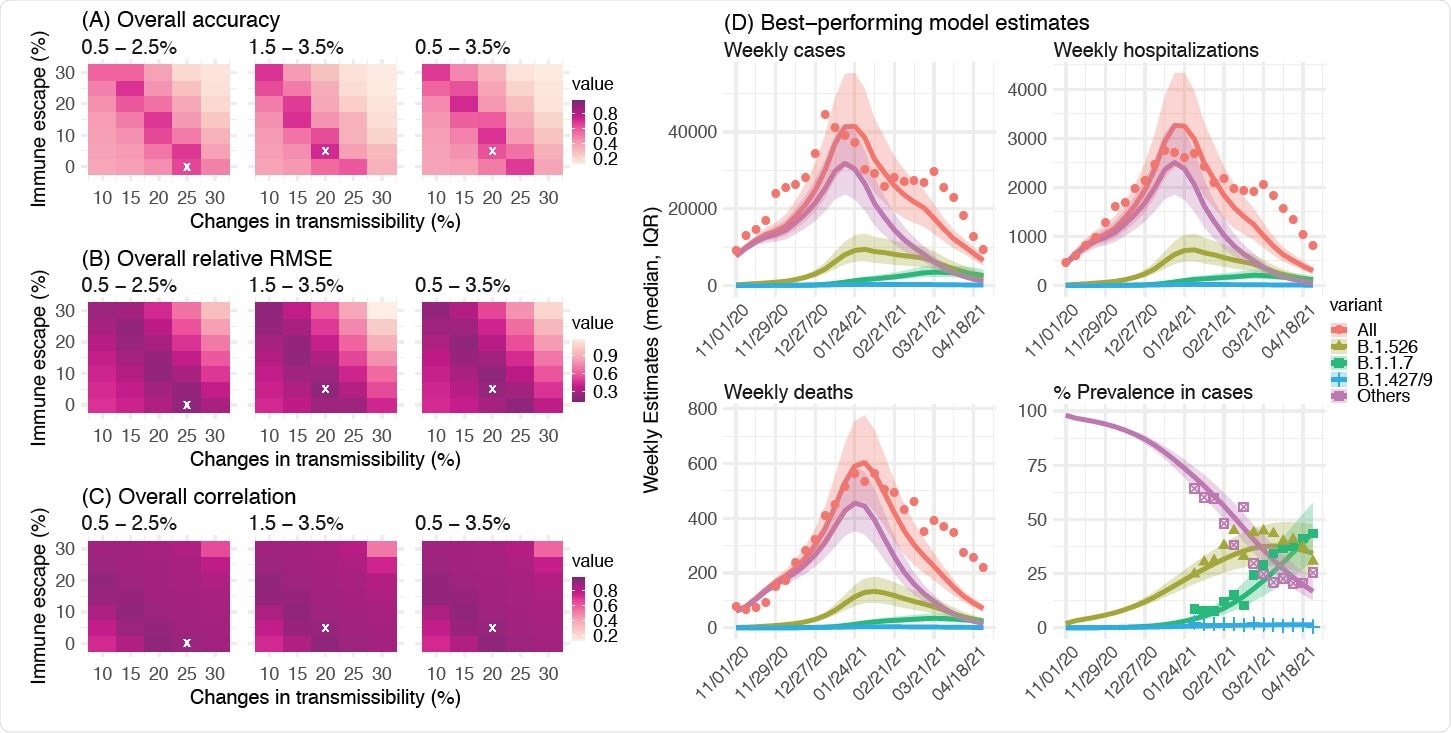
The scientists utilized a network model-inference system to estimate the transmission dynamics of SARS-CoV-2 and population-level variables and parameters in New York City. Based on collected information, they conducted a city-level multi-variant, age-structured modeling analysis to estimate the infection and immune evasion ability changes for the B.1.526 variant. The final analysis utilized the data obtained from two models to estimate the variant-specific mortality rate among individuals infected with SARS-CoV-2 (infection fatality risk).
For the network model-inference system, they utilized multiple epidemiological datasets as well as vaccination datasets. Similarly, the multi-variant model analysis utilized four weekly datasets, including confirmed and suspected COVID-19 cases, hospitalizations, mortality, and percentage of different SARS-CoV-2 variants circulating in New York City.
Important observations
In New York City, the population-level prevalence of SARS-CoV-2 infection was estimated to be 16.6% at the end of the first pandemic wave. Similarly, at the end of the second wave, the estimated prevalence was 41.7%. While most infections occurred in the older population during the first wave, the second wave caused infections in all age groups.
News
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
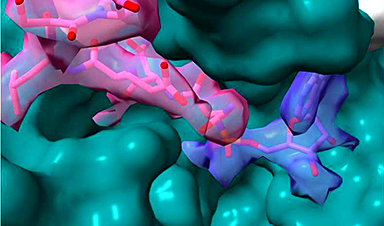
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
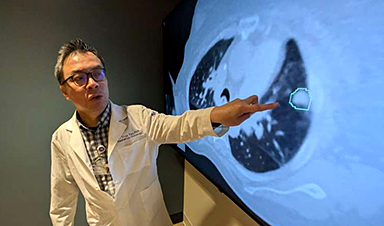
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]