Graphene is a layer of carbon only one atom thick. Since it was first isolated in 2004, it has found applications in strengthening materials, accelerating electronics, and boosting performance in batteries, among others.
It also shows great potential for use in biosensors. These are devices used to detect small concentrations of biomarkers in biological samples, such as blood or saliva. Biomarkers are molecules that suggest the presence of disease.
In a recent review, my colleagues and I looked into the latest research to find the most exciting potential applications of graphene in point-of-care tests. This includes diagnostic tests for SARS-CoV-2, the virus responsible for COVID-19, but also detecting other viruses, bacteria and even cancerous tumours.
It’s early days. The technology still needs to go through clinical trials and processes need to be developed to manufacture these tests at scale. However, in the next five years, graphene could start to play a part in healthcare technology.
A single atom layer
Because graphene is a two-dimensional material, it has a tremendously high surface-to-volume ratio, which makes it very sensitive to changes in its environment. Think of a vast, calm lake. Any tiny pebble that hits the surface creates a ripple that quickly expands across the water.
Similarly, when other substances—even single molecules—hit graphene, they generate small, measurable electrical pulses.
Relying on this phenomenon alone to detect SARS-CoV-2 wouldn’t work. When used as a biosensing layer in electronic devices, graphene is sensitive down to a single molecule. Yet it can’t tell the difference between coronavirus and the flu—the same way the lake would confuse a pebble and a marble.
To solve this, researchers have developed chemically modified graphene, coating it with antibodies that bind specifically to SARS-CoV-2. When the virus reaches the sensor and attaches to the antibody, it triggers an electrical signal through the thin graphene layer.
SARS-CoV-2 carries all its genetic information in a strand of RNA, which is often used in detection processes like a polymerase chain reaction (PCR). A PCR device amplifies the amount of RNA in a saliva sample until it becomes detectable under a microscope.
But this process is time consuming, requires expensive equipment and very specific and expensive reagents—substances used in the labelling and amplification process, or in the preparation of the sample.
Image Credit: Shutterstock
Post by Amanda Scott, NA CEO. Follow her on twitter @tantriclens
Thanks to Heinz V. Hoenen. Follow him on twitter: @HeinzVHoenen
News
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
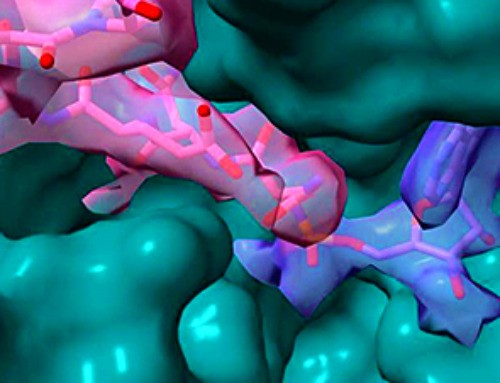
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
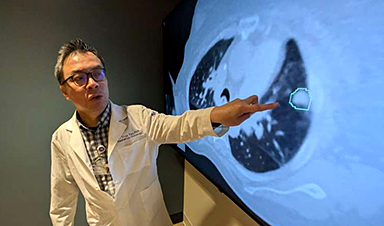
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]