Researchers discovered that during the COVID-19 pandemic, there was a surge in a rare autoimmune disease among previously unaffected demographic groups, leading to the deaths of nine patients.
COVID-19 as a Trigger for Autoimmune Response
The rise in cases is believed to be triggered by exposure to the COVID-19 virus. This condition manifests through distinctive skin rashes, pneumonia, and interstitial lung disease—a rapidly progressing type of lung inflammation that is often fatal.
“Whilst we very occasionally see this disease in the UK, this surge in cases was completely new and very different,” said Principal Investigator Dennis McGonagle, Professor of Investigative Rheumatology at the University of Leeds.
“It is important that physicians understand the symptoms so that patients can be quickly referred for treatment and have the best chance of a rapid and full recovery. Lives could undoubtedly be saved but there is a great need for research to try and slow or stop the rapid lung progression that occurs in some patients,” he adds.
Understanding MDA5 and Autoimmune Response
The immune system contains a protein called MDA5, which helps detect RNA viruses like COVID-19. Normally, this protein helps trigger an immune response in the body, where more of the protein is produced to help fight off the virus. However, sometimes the immune system releases antibodies that mistakenly attack this protein, leading to MDA5 autoimmune diseases such as the rare disease described in this study. The exact cause is not well understood, but scientists believe the virus itself could trigger the response. Autoimmune diseases seen after viral infections have similar features, such as fatigue, joint pain and swelling, skin rashes, and digestive issues.
Case Study and Analysis
The 60 patients in the study presented at their GPs or to A&E with a range of symptoms including shortness of breath, muscle pain, rashes, and reduced blood flow to the fingers, known as Raynaud’s disease. These symptoms are associated with autoimmune disease.
The patients were referred to rheumatology specialists for further testing and all were diagnosed with the condition. Of the 60 patients, 35 had received COVID-19 vaccinations, and 15 had previously tested positive for COVID-19. However, patients were not systematically tested for COVID-19, and some may have been infected, but were asymptomatic at the time. Such cases could have developed MDA5 disease due to an overreaction of their immune system to minimal exposure to the virus.
Twenty-five out of the 60 patients (41.7%) developed interstitial lung disease, and despite treatment with immunosuppressant medication, eight of those patients died. A ninth patient, who did not have interstitial lung disease, died from sepsis.
To understand the increase in cases of this rare condition, researchers collected data on the number of these tests between January 2018 and December 2022, alongside data on COVID-19 infections and vaccination, and information about each patient’s symptoms. Analysis showed that just six cases of the rare condition had been diagnosed between 2018 and 2019. However, in the 3 years after 60 new cases appeared, eight cases were diagnosed in 2020; 35 cases were diagnosed in 2021 and 17 cases were diagnosed in 2022. Very few cases have occurred since then.
Patient Demographics and Observations
Patients ranged in age from 43 to 71, with 36 of them being female.
Ethnicity:
- White: 32
- South Asian: 3
- Black Caribbean: 2
- Black African: 1
- Any other ethnic group: 4
- Asian (not Chinese): 4
- There was no ethnicity data for 14 patients.
Researchers noted that there was a strong overlap in 2021 between vaccination rates in Yorkshire and the surge in MDA5 disease cases. This peak, though, also occurred shortly after a community wave of coronavirus infection occurred in late 2021. A smaller overlap was seen between confirmed COVID-19 infection and MDA5. However, it was interesting to note that almost half (42%) of patients were not documented to have been vaccinated against COVID-19 before they tested positive for MDA5. Four children who tested positive for MDA5 were unvaccinated, pointing to the idea of an overreacting immune response after exposure to a virus.
McGonagle said: “We know that vaccines can trigger an immune overreaction, but given that not all of these patients were vaccinated against COVID-19, and the increase in cases occurred when the COVID-19 virus was circulating in significant numbers, the evidence strongly suggests that the increase in cases of this rare disease is linked to exposure to the virus.”
This work was done in collaboration with Dr Pradipta Ghosh and her team at the University of California, San Diego, who showed that the MDA5 protein was found in higher amounts in patients with COVID-19 and in patients with other diseases involving MDA5. They discovered that this increase was linked to an abnormal immune response that slows the virus’s ability to multiply and spread. Additionally, they found that higher levels of the MDA5 protein were associated with increased levels of Interleukin-15, a protein that activates T-cells, or immune cells. This interaction could be contributing to the autoimmune response.
Impact and Significance of Research
The study highlights the critical need for awareness among doctors about this condition to ensure prompt diagnosis and treatment, which could mitigate lung damage and save lives. This is especially so in subjects with suspected pneumonia not getting better on therapy and where the rashes, muscle involvement, and other disease features are absent.
“We think that this large, unprecedented outbreak of MDA5 disease in Yorkshire will help advance the field to better appreciate the role between viruses and autoimmunity,” said Dr Paula David, the lead author of the study.
Dr. Saptarshi Sinha, the co-first author of the paper and the interim director of PreCSN, added: “Here at PreCSN, we enjoy the ability to help researchers such as the McGonagle group dive into big data and find patterns rapidly with precision that allows us to connect the dots. In this case, we are glad we could find a connection between a clinical presentation of autoimmune disease in the backdrop of COVID-19 at a molecular level.”
For more on this study, see Entirely New COVID-Related Syndrome Discovered.
Reference: “MDA5-autoimmunity and interstitial pneumonitis contemporaneous with the COVID-19 pandemic (MIP-C)” by Paula David, Saptarshi Sinha, Khizer Iqbal, Gabriele De Marco, Sahar Taheri, Ella McLaren, Sheetal Maisuria, Gururaj Arumugakani, Zoe Ash, Catrin Buckley, Lauren Coles, Chamila Hettiarachchi, Emma Payne, Sinisa Savic, Gayle Smithson, Maria Slade, Rahul Shah, Helena Marzo-Ortega, Mansoor Keen, Catherine Lawson, Joanna Mclorinan, Sharmin Nizam, Hanu Reddy, Omer Sharif, Shabina Sultan, Gui Tran, Mark Wood, Samuel Wood, Pradipta Ghosh and Dennis McGonagle, 8 May 2024, eBioMedicine.
DOI: 10.1016/j.ebiom.2024.105136
The data was generated by Dr Paula David and Dr Gabriele DeMarco from the University of Leeds’ School of Medicine and the Leeds Teaching Hospitals NHS Trust, with their Trust colleague Dr Khizer Iqbal.
News
Nano-Enhanced Hydrogel Strategies for Cartilage Repair
A recent article in Engineering describes the development of a protein-based nanocomposite hydrogel designed to deliver two therapeutic agents—dexamethasone (Dex) and kartogenin (KGN)—to support cartilage repair. The hydrogel is engineered to modulate immune responses and promote [...]
New Cancer Drug Blocks Tumors Without Debilitating Side Effects
A new drug targets RAS-PI3Kα pathways without harmful side effects. It was developed using high-performance computing and AI. A new cancer drug candidate, developed through a collaboration between Lawrence Livermore National Laboratory (LLNL), BridgeBio Oncology [...]
Scientists Are Pretty Close to Replicating the First Thing That Ever Lived
For 400 million years, a leading hypothesis claims, Earth was an “RNA World,” meaning that life must’ve first replicated from RNA before the arrival of proteins and DNA. Unfortunately, scientists have failed to find [...]
Why ‘Peniaphobia’ Is Exploding Among Young People (And Why We Should Be Concerned)
An insidious illness is taking hold among a growing proportion of young people. Little known to the general public, peniaphobia—the fear of becoming poor—is gaining ground among teens and young adults. Discover the causes [...]
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
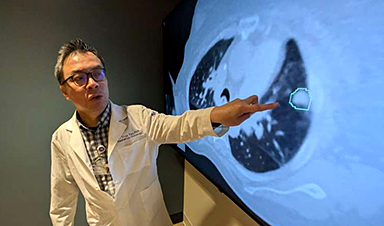
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]