Researchers in Japan found that although the Alzheimer's drug lecanemab successfully removes amyloid plaques from the brain, it does not restore the brain's waste-clearing system within the first few months of treatment.
The study suggests that by the time symptoms appear, damage to nerve cells and the glymphatic system is already well established, making short-term recovery unlikely.
Lecanemab's Surprising Limits in Alzheimer's Treatment
Researchers at Osaka Metropolitan University in Japan, led by graduate student Tatsushi Oura and Dr. Hiroyuki Tatekawa, reported that lecanemab, a drug designed to clear amyloid plaques from the brain, does not improve the brain's waste removal system in the early stages after treatment.
Their results indicate that the nerves of Alzheimer's disease (AD) patients have already sustained considerable damage, and that this waste-clearing function does not rebound quickly. The findings point to the need for treatments that target several biological problems at the same time.
The Complex Web of Alzheimer's Disease Mechanisms
The researchers' results add another piece to the long and complicated effort to understand how AD develops. Although it is the most widespread neurodegenerative disorder, it remains difficult to treat because many different factors contribute to its progression.
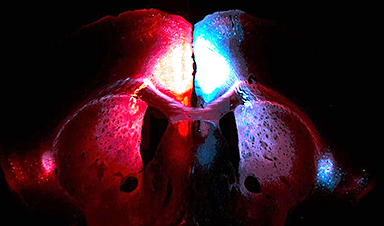
A major driver of nerve cell damage in AD is the accumulation of amyloid-β (Aβ) in the brain. In people without the disease, a network known as the glymphatic system circulates cerebrospinal fluid along the spaces surrounding arteries and into brain tissue. There, this fluid mixes with interstitial fluid to help remove metabolic waste products, including Aβ. The name "glymphatic system" comes from the involvement of glial cells in this process.
In AD, however, Aβ builds up and causes arteries to stiffen. This reduces the movement of fluid between the brain and the cerebrospinal fluid, which disrupts waste removal and leads to a series of harmful changes that produce AD symptoms.
Testing Lecanemab's Effects on Brain Clearance
Lecanemab, which was recently approved as a therapeutic option, is intended to lower Aβ levels. To study its effects, the Osaka Metropolitan University team examined the glymphatic system in patients both before and after lecanemab treatment, using the DTI-ALPS index to measure changes.
They found no meaningful difference in this index when comparing pre-treatment results with measurements taken three months after therapy.
What This Means for Future Alzheimer's Treatments
Based on these observations, the researchers concluded that while anti-amyloid drugs can reduce plaque buildup and slow additional cognitive decline, they may not be able to restore functions already lost. By the time symptoms appear, many patients likely have long-standing neuronal damage and glymphatic impairment that are difficult to reverse. The results emphasize how many interconnected factors drive AD and how few of them can be quickly repaired.
"Even when Aβ is reduced by lecanemab, impairment of the glymphatic system may not recover within the short-term," Oura said. "In the future, we want to look at factors like age, the stage of the disease, and degree of lesions in the white matter to further understand the relationship between changes in the glymphatic system due to lecanemab treatment and the outcome of treatment. This will help understand the best way to administer treatment to patients."
Reference: "Unchanged Early Diffusion Tensor Imaging Along Perivascular Space Index After Amyloid-Targeting Disease-Modifying Therapy in Alzheimer's Disease: A Preliminary Study" by Tatsushi Oura, Hiroyuki Tatekawa, Akitoshi Takeda, Ayako Omori, Natsuko Atsukawa, Shu Matsushita, Daisuke Horiuchi, Hirotaka Takita, Taro Shimono, Daiju Ueda, Yoshiaki Itoh and Yukio Miki, 8 September 2025, Journal of Magnetic Resonance Imaging.
DOI: 10.1002/jmri.70118
The study was published in Journal of Magnetic Resonance Imaging.
News
This Is Why the Same Virus Hits People So Differently
Scientists have mapped how genetics and life experiences leave lasting epigenetic marks on immune cells. The discovery helps explain why people respond so differently to the same infections and could lead to more personalized [...]
Rejuvenating neurons restores learning and memory in mice
EPFL scientists report that briefly switching on three “reprogramming” genes in a small set of memory-trace neurons restored memory in aged mice and in mouse models of Alzheimer’s disease to level of healthy young [...]
New book from Nanoappsmedical Inc. – Global Health Care Equivalency
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
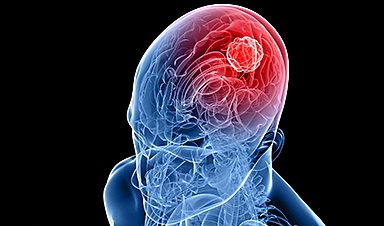
New Molecule Blocks Deadliest Brain Cancer at Its Genetic Root
Researchers have identified a molecule that disrupts a critical gene in glioblastoma. Scientists at the UVA Comprehensive Cancer Center say they have found a small molecule that can shut down a gene tied to glioblastoma, a [...]
Scientists Finally Solve a 30-Year-Old Cancer Mystery Hidden in Rye Pollen
Nearly 30 years after rye pollen molecules were shown to slow tumor growth in animals, scientists have finally determined their exact three-dimensional structures. Nearly 30 years ago, researchers noticed something surprising in rye pollen: [...]
NanoMedical Brain/Cloud Interface – Explorations and Implications. A new book from Frank Boehm
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
How lipid nanoparticles carrying vaccines release their cargo
A study from FAU has shown that lipid nanoparticles restructure their membrane significantly after being absorbed into a cell and ending up in an acidic environment. Vaccines and other medicines are often packed in [...]
New book from NanoappsMedical Inc – Molecular Manufacturing: The Future of Nanomedicine
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
A Virus Designed in the Lab Could Help Defeat Antibiotic Resistance
Scientists can now design bacteria-killing viruses from DNA, opening a faster path to fighting superbugs. Bacteriophages have been used as treatments for bacterial infections for more than a century. Interest in these viruses is rising [...]
Sleep Deprivation Triggers a Strange Brain Cleanup
When you don’t sleep enough, your brain may clean itself at the exact moment you need it to think. Most people recognize the sensation. After a night of inadequate sleep, staying focused becomes harder [...]
Lab-grown corticospinal neurons offer new models for ALS and spinal injuries
Researchers have developed a way to grow a highly specialized subset of brain nerve cells that are involved in motor neuron disease and damaged in spinal injuries. Their study, published today in eLife as the final [...]
Urgent warning over deadly ‘brain swelling’ virus amid fears it could spread globally
Airports across Asia have been put on high alert after India confirmed two cases of the deadly Nipah virus in the state of West Bengal over the past month. Thailand, Nepal and Vietnam are among the [...]
This Vaccine Stops Bird Flu Before It Reaches the Lungs
A new nasal spray vaccine could stop bird flu at the door — blocking infection, reducing spread, and helping head off the next pandemic. Since first appearing in the United States in 2014, H5N1 [...]
These two viruses may become the next public health threats, scientists say
Two emerging pathogens with animal origins—influenza D virus and canine coronavirus—have so far been quietly flying under the radar, but researchers warn conditions are ripe for the viruses to spread more widely among humans. [...]
COVID-19 viral fragments shown to target and kill specific immune cells
COVID-19 viral fragments shown to target and kill specific immune cells in UCLA-led study Clues about extreme cases and omicron’s effects come from a cross-disciplinary international research team New research shows that after the [...]
Smaller Than a Grain of Salt: Engineers Create the World’s Tiniest Wireless Brain Implant
A salt-grain-sized neural implant can record and transmit brain activity wirelessly for extended periods. Researchers at Cornell University, working with collaborators, have created an extremely small neural implant that can sit on a grain of [...]