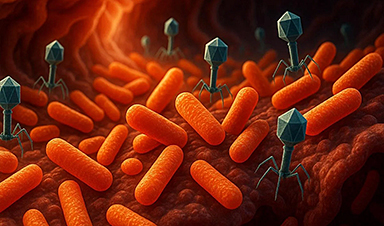
Scientists have long known that bacteriophages, viruses that infect bacteria, live in our gut, but exactly what they do has remained elusive.
Researchers developed a clever mouse model that can temporarily eliminate these phages without harming the bacteria, using a UTI treatment ingredient called acriflavine. Their experiments showed that without phages, gut bacteria become less sensitive to antibiotics, suggesting that these tiny viruses might actually worsen the microbiome damage antibiotics cause. This surprising connection could lead to new breakthroughs in gut health research.
Gut Viruses: The Overlooked Partners of Bacteria
Some things are just meant to be together: peanut butter and jelly, salt and pepper — and in your gut, bacteria and the viruses that infect them.
These viruses, known as bacteriophages, naturally target the bacterial species living in your digestive system. Although phages have evolved alongside bacteria for millions of years, they remain far less understood. They're tricky to classify and so closely intertwined with their bacterial hosts that scientists still aren't sure exactly what roles they play.
But what if researchers could compare a gut microbiome with and without these viruses, under otherwise identical conditions?
A New Way to Study Phages
At Virginia Tech, biologist Bryan Hsu and his team figured out how to do just that.
Hsu and graduate student Hollyn Franklin developed a model that can selectively remove bacteriophages from a mouse's gut microbiome — and later restore them — without disturbing the bacteria themselves. In early tests of the model, the researchers found intriguing evidence that phages might actually make gut bacteria more sensitive to antibiotics. Their findings were published today (April 28) in the journal Cell Host & Microbe.
Acriflavine: The Phage-Silencing Compound
What could inhibit a bacteria's viruses but not the bacteria itself? In her early search through the literature, Franklin found a chemical compound called acriflavine that fit the bill. It's a component of a widely available medication used in Brazil to treat urinary tract infections (UTI).
Fortuitously, a member of Hsu's lab and paper co-author, Rogerio Bataglioli, is a native Brazilian. He shipped a massive order of acriflavine to his parent's house. But he forgot to tell his parents it was coming, Hsu said.
"His mom called, and asked, 'Is everything OK? Because 20 boxes of UTI treatment just arrived under your name.'"
From UTI Medicine to Breakthrough Experiment
After that was sorted, Franklin began administering acriflavine to lab mice. Over a period of 12 days, there was a dramatic reduction in the concentration of viral particles. And they didn't bounce back when she stopped administering the drug.
But when Franklin reintroduced a tiny sample of the mouse's own gut microbiome, extracted before treatment, the natural phage populations sprang back to life.
"It went away when we wanted it to, and came back when we wanted it to," said Hsu. "Which means we have a bacteriophage conditional mouse model."
Or, more fun: BaCon mouse model.
The Power of a Switchable Microbiome
To see if the mouse model had some significance for health, Hsu's research team went straight to one of the hottest topics in the field: the collateral damage that antibiotics have on a patient's resident microbial population.
Antibiotics save millions of lives every year, but the drug rages indiscriminately through bad, benign, and beneficial bacteria alike, disrupting our gut microbiome and leaving us vulnerable to new pathogens.
Antibiotics, Gut Microbes, and Phage Interference
Could phages be playing a role in the destructive wake of an antibiotic treatment? Hsu and Franklin used their BaCon mouse model to ask this question and administered antibiotics to mice with and without phage populations.
Their results suggest that phages increase the sensitivity of bacteria to antibiotics.
"It's hard to make definitive conclusions, but these results are telling us that phages have some significance for how we respond to antibiotics," Hsu said.
Phages: Potential Game Changers in Microbiome Health
The next questions, according to Franklin, will explore if phages caused these effects or are simply correlated with them, and what role phages play in diseases, which would open new doors in microbiome studies.
Answers may be served with a side of BaCon mouse.
Reference: 28 April 2025, Cell Host & Microbe.
Funding for this work was provided by the Virginia Tech Institute for Critical Technology and Applied Science, the National Institute of General Medical Sciences of the National Institutes of Health.
Research collaborators include:
- Frank Aylward, associate professor of biological sciences
- Anh Ha, postdoctoral research associate
- Rita Makhlouf, graduate student, biological sciences
- Zachary Baker, graduate student, biological sciences
- Sydney Murphy ´24, former undergraduate researcher in the Hsu Lab
- Hannah Jirsa ´23, former undergraduate researcher in the Hsu Lab
- Joshua Heuler, graduate student, biological sciences
- Teresa Southard, associate professor of anatomic pathology
News
Smaller Than a Grain of Salt: Engineers Create the World’s Tiniest Wireless Brain Implant
A salt-grain-sized neural implant can record and transmit brain activity wirelessly for extended periods. Researchers at Cornell University, working with collaborators, have created an extremely small neural implant that can sit on a grain of [...]
Scientists Develop a New Way To See Inside the Human Body Using 3D Color Imaging
A newly developed imaging method blends ultrasound and photoacoustics to capture both tissue structure and blood-vessel function in 3D. By blending two powerful imaging methods, researchers from Caltech and USC have developed a new way to [...]
Brain waves could help paralyzed patients move again
People with spinal cord injuries often lose the ability to move their arms or legs. In many cases, the nerves in the limbs remain healthy, and the brain continues to function normally. The loss of [...]
Scientists Discover a New “Cleanup Hub” Inside the Human Brain
A newly identified lymphatic drainage pathway along the middle meningeal artery reveals how the human brain clears waste. How does the brain clear away waste? This task is handled by the brain’s lymphatic drainage [...]
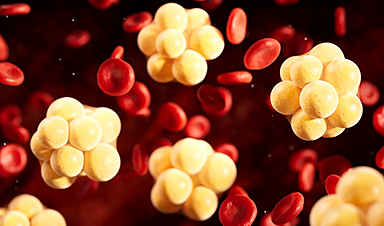
New Drug Slashes Dangerous Blood Fats by Nearly 40% in First Human Trial
Scientists have found a way to fine-tune a central fat-control pathway in the liver, reducing harmful blood triglycerides while preserving beneficial cholesterol functions. When we eat, the body turns surplus calories into molecules called [...]
A Simple Brain Scan May Help Restore Movement After Paralysis
A brain cap and smart algorithms may one day help paralyzed patients turn thought into movement—no surgery required. People with spinal cord injuries often experience partial or complete loss of movement in their arms [...]
Plant Discovery Could Transform How Medicines Are Made
Scientists have uncovered an unexpected way plants make powerful chemicals, revealing hidden biological connections that could transform how medicines are discovered and produced. Plants produce protective chemicals called alkaloids as part of their natural [...]
Scientists Develop IV Therapy That Repairs the Brain After Stroke
New nanomaterial passes the blood-brain barrier to reduce damaging inflammation after the most common form of stroke. When someone experiences a stroke, doctors must quickly restore blood flow to the brain to prevent death. [...]
Analyzing Darwin’s specimens without opening 200-year-old jars
Scientists have successfully analyzed Charles Darwin's original specimens from his HMS Beagle voyage (1831 to 1836) to the Galapagos Islands. Remarkably, the specimens have been analyzed without opening their 200-year-old preservation jars. Examining 46 [...]
Scientists discover natural ‘brake’ that could stop harmful inflammation
Researchers at University College London (UCL) have uncovered a key mechanism that helps the body switch off inflammation—a breakthrough that could lead to new treatments for chronic diseases affecting millions worldwide. Inflammation is the [...]
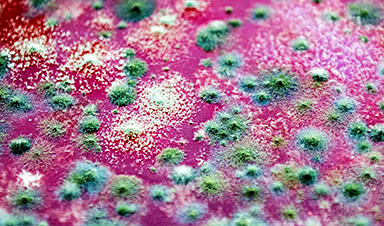
A Forgotten Molecule Could Revive Failing Antifungal Drugs and Save Millions of Lives
Scientists have uncovered a way to make existing antifungal drugs work again against deadly, drug-resistant fungi. Fungal infections claim millions of lives worldwide each year, and current medical treatments are failing to keep pace. [...]
Scientists Trap Thyme’s Healing Power in Tiny Capsules
A new micro-encapsulation breakthrough could turn thyme’s powerful health benefits into safer, smarter nanodoses. Thyme extract is often praised for its wide range of health benefits, giving it a reputation as a natural medicinal [...]
Scientists Develop Spray-On Powder That Instantly Seals Life-Threatening Wounds
KAIST scientists have created a fast-acting, stable powder hemostat that stops bleeding in one second and could significantly improve survival in combat and emergency medicine. Severe blood loss remains the primary cause of death from [...]
Oceans Are Struggling To Absorb Carbon As Microplastics Flood Their Waters
New research points to an unexpected way plastic pollution may be influencing Earth’s climate system. A recent study suggests that microscopic plastic pollution is reducing the ocean’s capacity to take in carbon dioxide, a [...]
Molecular Manufacturing: The Future of Nanomedicine – New book from Frank Boehm
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
New Book! NanoMedical Brain/Cloud Interface – Explorations and Implications
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]