By providing plausible label maps for one medical image, the Tyche machine-learning model could help clinicians and researchers capture crucial information.
In biomedicine, segmentation involves annotating pixels from an important structure in a medical image, like an organ or cell. Artificial intelligence models can help clinicians by highlighting pixels that may show signs of a certain disease or anomaly.
However, these models typically only provide one answer, while the problem of medical image segmentation is often far from black and white. Five expert human annotators might provide five different segmentations, perhaps disagreeing on the existence or extent of the borders of a nodule in a lung CT image.
Embracing Uncertainty in Diagnosis
“Having options can help in decision-making. Even just seeing that there is uncertainty in a medical image can influence someone’s decisions, so it is important to take this uncertainty into account,” says Marianne Rakic, an MIT computer science PhD candidate.
Rakic is lead author of a paper with others at MIT, the Broad Institute of MIT and Harvard, and Massachusetts General Hospital that introduces a new AI tool that can capture the uncertainty in a medical image.
Introduction of Tyche
Known as Tyche (named for the Greek divinity of chance), the system provides multiple plausible segmentations that each highlight slightly different areas of a medical image. A user can specify how many options Tyche outputs and select the most appropriate one for their purpose.
Importantly, Tyche can tackle new segmentation tasks without needing to be retrained. Training is a data-intensive process that involves showing a model many examples and requires extensive machine-learning experience.
Because it doesn’t need retraining, Tyche could be easier for clinicians and biomedical researchers to use than some other methods. It could be applied “out of the box” for a variety of tasks, from identifying lesions in a lung X-ray to pinpointing anomalies in a brain MRI.
Ultimately, this system could improve diagnoses or aid in biomedical research by calling attention to potentially crucial information that other AI tools might miss.
“Ambiguity has been understudied. If your model completely misses a nodule that three experts say is there and two experts say is not, that is probably something you should pay attention to,” adds senior author Adrian Dalca, an assistant professor at Harvard Medical School and MGH, and a research scientist in the MIT Computer Science and Artificial Intelligence Laboratory (CSAIL).
Their co-authors include Hallee Wong, a graduate student in electrical engineering and computer science; Jose Javier Gonzalez Ortiz PhD ’23; Beth Cimini, associate director for bioimage analysis at the Broad Institute; and John Guttag, the Dugald C. Jackson Professor of Computer Science and Electrical Engineering. Rakic will present Tyche at the IEEE Conference on Computer Vision and Pattern Recognition, where Tyche has been selected as a highlight.
Addressing Ambiguity With AI
AI systems for medical image segmentation typically use neural networks. Loosely based on the human brain, neural networks are machine-learning models comprising many interconnected layers of nodes, or neurons, that process data.
After speaking with collaborators at the Broad Institute and MGH who use these systems, the researchers realized two major issues limit their effectiveness. The models cannot capture uncertainty and they must be retrained for even a slightly different segmentation task.
Some methods try to overcome one pitfall, but tackling both problems with a single solution has proven especially tricky, Rakic says.
“If you want to take ambiguity into account, you often have to use an extremely complicated model. With the method we propose, our goal is to make it easy to use with a relatively small model so that it can make predictions quickly,” she says.
The researchers built Tyche by modifying a straightforward neural network architecture.
A user first feeds Tyche a few examples that show the segmentation task. For instance, examples could include several images of lesions in a heart MRI that have been segmented by different human experts so the model can learn the task and see that there is ambiguity.
The researchers found that just 16 example images, called a “context set,” is enough for the model to make good predictions, but there is no limit to the number of examples one can use. The context set enables Tyche to solve new tasks without retraining.
For Tyche to capture uncertainty, the researchers modified the neural network so it outputs multiple predictions based on one medical image input and the context set. They adjusted the network’s layers so that, as data move from layer to layer, the candidate segmentations produced at each step can “talk” to each other and the examples in the context set.
In this way, the model can ensure that candidate segmentations are all a bit different, but still solve the task.
“It is like rolling dice. If your model can roll a two, three, or four, but doesn’t know you have a two and a four already, then either one might appear again,” she says.
They also modified the training process so it is rewarded by maximizing the quality of its best prediction.
If the user asked for five predictions, at the end they can see all five medical image segmentations Tyche produced, even though one might be better than the others.
The researchers also developed a version of Tyche that can be used with an existing, pretrained model for medical image segmentation. In this case, Tyche enables the model to output multiple candidates by making slight transformations to images.
Better, Faster Predictions
When the researchers tested Tyche with datasets of annotated medical images, they found that its predictions captured the diversity of human annotators, and that its best predictions were better than any from the baseline models. Tyche also performed faster than most models.
“Outputting multiple candidates and ensuring they are different from one another really gives you an edge,” Rakic says.
The researchers also saw that Tyche could outperform more complex models that have been trained using a large, specialized dataset.
For future work, they plan to try using a more flexible context set, perhaps including text or multiple types of images. In addition, they want to explore methods that could improve Tyche’s worst predictions and enhance the system so it can recommend the best segmentation candidates.
Reference: “Tyche: Stochastic In-Context Learning for Medical Image Segmentation” by Marianne Rakic, Hallee E. Wong, Jose Javier Gonzalez Ortiz, Beth Cimini, John Guttag and Adrian V. Dalca, 24 January 2024, Electrical Engineering and Systems Science > Image and Video Processing.
arXiv:2401.13650
This research is funded, in part, by the National Institutes of Health, the Eric and Wendy Schmidt Center at the Broad Institute of MIT and Harvard, and Quanta Computer.
News
The Silent Battle Within: How Your Organs Choose Between Mom and Dad’s Genes
Research reveals that selective expression of maternal or paternal X chromosomes varies by organ, driven by cellular competition. A new study published today (July 26) in Nature Genetics by the Lymphoid Development Group at the MRC [...]
Study identifies genes increasing risk of severe COVID-19
Whether or not a person becomes seriously ill with COVID-19 depends, among other things, on genetic factors. With this in mind, researchers from the University Hospital Bonn (UKB) and the University of Bonn, in [...]
Small regions of the brain can take micro-naps while the rest of the brain is awake and vice versa
Sleep and wake: They're totally distinct states of being that define the boundaries of our daily lives. For years, scientists have measured the difference between these instinctual brain processes by observing brain waves, with [...]
Redefining Consciousness: Small Regions of the Brain Can Take Micro-Naps While the Rest of the Brain Is Awake
The study broadly reveals how fast brain waves, previously overlooked, establish fundamental patterns of sleep and wakefulness. Scientists have developed a new method to analyze sleep and wake states by detecting ultra-fast neuronal activity [...]
AI Reveals Health Secrets Through Facial Temperature Mapping
Researchers have found that different facial temperatures correlate with chronic illnesses like diabetes and high blood pressure, and these can be detected using AI with thermal cameras. They highlight the potential of this technology [...]
Breakthrough in aging research: Blocking IL-11 extends lifespan and improves health in mice
In a recent study published in the journal Nature, a team of researchers used murine models and various pharmacological and genetic approaches to examine whether pro-inflammatory signaling involving interleukin (IL)-11, which activates signaling molecules such [...]
Promise for a universal influenza vaccine: Scientists validate theory using 1918 flu virus
New research led by Oregon Health & Science University reveals a promising approach to developing a universal influenza vaccine—a so-called "one and done" vaccine that confers lifetime immunity against an evolving virus. The study, [...]
New Projects Aim To Pioneer the Future of Neuroscience
One study will investigate the alterations in brain activity at the cellular level caused by psilocybin, the psychoactive substance found in “magic mushrooms.” How do neurons respond to the effects of magic mushrooms? What [...]
Decoding the Decline: Scientific Insights Into Long COVID’s Retreat
Research indicates a significant reduction in long COVID risk, largely due to vaccination and the virus’s evolution. The study analyzes data from over 441,000 veterans, showing lower rates of long COVID among vaccinated individuals compared [...]
Silicon Transformed: A Breakthrough in Laser Nanofabrication
A new method enables precise nanofabrication inside silicon using spatial light modulation and laser pulses, creating advanced nanostructures for potential use in electronics and photonics. Silicon, the cornerstone of modern electronics, photovoltaics, and photonics, [...]
Caught in the actinium: New research could help design better cancer treatments
The element actinium was first discovered at the turn of the 20th century, but even now, nearly 125 years later, researchers still don't have a good grasp on the metal's chemistry. That's because actinium [...]
Innovative Light-Controlled Drugs Could Revolutionize Neuropathic Pain Treatment
A team of researchers from the Institute for Bioengineering of Catalonia (IBEC) has developed light-activated derivatives of the anti-epileptic drug carbamazepine to treat neuropathic pain. Light can be harnessed to target drugs to specific [...]
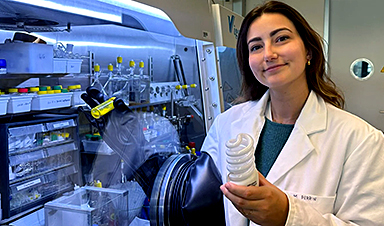
Green Gold: Turning E-Waste Into a Treasure Trove of Rare Earth Metals
Scientists are developing a process inspired by nature that efficiently recovers europium from old fluorescent lamps. The approach could lead to the long-awaited recycling of rare earth metals. A small molecule that naturally serves [...]
Cambridge Study: AI Chatbots Have an “Empathy Gap,” and It Could Be Dangerous
A new study suggests a framework for “Child Safe AI” in response to recent incidents showing that many children perceive chatbots as quasi-human and reliable. A study has indicated that AI chatbots often exhibit [...]
Nanoparticle-based delivery system could offer treatment for diabetics with rare insulin allergy
Up to 3% of people with diabetes have an allergic reaction to insulin. A team at Forschungszentrum Jülich has now studied a method that could be used to deliver the active substance into the [...]
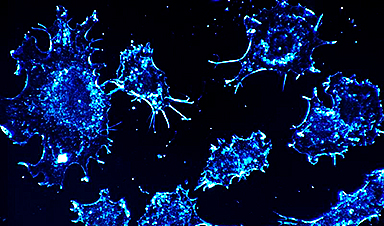
Nanorobot kills cancer cells in mice with hidden weapon
Researchers at Karolinska Institutet in Sweden have developed nanorobots that kill cancer cells in mice. The robot's weapon is hidden in a nanostructure and is exposed only in the tumor microenvironment, sparing healthy cells. [...]