Experimental mRNA vaccine proves highly effective against H5N1 in animal studies, offering hope for rapid pandemic response.
Researchers from the Perelman School of Medicine at the University of Pennsylvania have developed an experimental mRNA vaccine against avian influenza virus H5N1. The vaccine is highly effective in preventing severe illness and death in preclinical models and could help manage the current H5N1 outbreaks in birds and cattle in the United States and prevent its transmission to humans.
This research was recently published in Nature Communications.
Advantages of mRNA Technology in Vaccine Development
Scott Hensley, PhD, a professor of Microbiology at the Perelman School of Medicine, highlighted the flexibility of mRNA technology in vaccine development. “The mRNA technology allows us to be much more agile in developing vaccines; we can start creating an mRNA vaccine within hours of sequencing a new viral strain with pandemic potential,” he explained.
“During previous influenza pandemics, like the 2009 H1N1 pandemic, vaccines were difficult to manufacture and did not become available until after the initial pandemic waves subsided.”
Hensley’s laboratory worked on this study in collaboration with the laboratory of mRNA vaccine pioneer and Nobel Prize winner Drew Weissman, MD, PhD.
“Before 2020, experts thought the influenza virus posed the greatest risk of causing a pandemic, and we had limited options for creating a vaccine if that had happened,” said Weissman. “COVID-19 showed us the power of mRNA-based vaccines as tool to protect humans from emerging viruses quickly, and we are better prepared now to respond to a variety of viruses with pandemic potential, including influenza”
Traditional vs. mRNA Vaccine Production
Most influenza vaccines are egg-based, where experts inject fertilized chicken eggs with what they predict will be the dominant viral strain, let it replicate, and then inactivate the virus to use in the flu shots distributed globally. However, viruses must first be adapted to replicate in fertilized eggs before these conventional vaccines can be produced, which can take up to six months, presenting potential problems for quickly producing vaccine when it’s needed most during the first few months of a pandemic. mRNA vaccines are easily and quickly adapted to protect against different strains of influenza viruses, and don’t require eggs for their development.
Study Findings and Vaccine Efficacy
The Penn researchers developed an mRNA vaccine targeting a specific subtype of the H5N1 virus that is circulating widely in birds and cattle. While it rarely infects humans, some fear that the virus may evolve and cause a human pandemic. The researchers found that the vaccine elicited a strong antibody and T-cell response in mice and ferrets. What’s more, the animals maintained high levels of antibodies even a year after vaccination. Additionally, the researchers found that vaccinated animals who were subsequently infected with H5N1 cleared the virus more rapidly and displayed fewer symptoms than unvaccinated controls. The researchers also note that all of the vaccinated animals survived following H5N1 infection, whereas all the unvaccinated animals died.
Finally, the researchers compared the mRNA vaccine response in mice to their response to a traditional egg-based vaccine and found that the mRNA vaccine was just as effective; both vaccines elicited strong antibody responses, regardless of prior seasonal flu exposures.
Reference: “Development of a nucleoside-modified mRNA vaccine against clade 2.3.4.4b H5 highly pathogenic avian influenza virus” by Colleen Furey, Gabrielle Scher, Naiqing Ye, Lisa Kercher, Jennifer DeBeauchamp, Jeri Carol Crumpton, Trushar Jeevan, Christopher Patton, John Franks, Adam Rubrum, Mohamad-Gabriel Alameh, Steven H. Y. Fan, Anthony T. Phan, Christopher A. Hunter, Richard J. Webby, Drew Weissman and Scott E. Hensley, 23 May 2024, Nature Communications.
DOI: 10.1038/s41467-024-48555-z
The Hunter Laboratory at the University of Pennsylvania School of Veterinary Medicine, the Webby Lab at St. Jude, and Steven Fan at Acuitas also contributed to this research.
This research was funded by the National Institute of Allergy and Infectious Diseases, the National Institutes of Health, and the Department of Health and Human Services (75N93021C00015, 75N93021C00016, R01AI08686, and R01AI126899).
News
Breakthrough in Antimicrobial Technology with Cinnamon-Based Nanokiller
The need for innovative antimicrobial agents has become increasingly urgent due to the rise of antibiotic-resistant pathogens and the persistent threat of infections acquired during hospital stays. Traditional antibiotics and antiseptics are often ineffective [...]
The Silent Battle Within: How Your Organs Choose Between Mom and Dad’s Genes
Research reveals that selective expression of maternal or paternal X chromosomes varies by organ, driven by cellular competition. A new study published today (July 26) in Nature Genetics by the Lymphoid Development Group at the MRC [...]
Study identifies genes increasing risk of severe COVID-19
Whether or not a person becomes seriously ill with COVID-19 depends, among other things, on genetic factors. With this in mind, researchers from the University Hospital Bonn (UKB) and the University of Bonn, in [...]
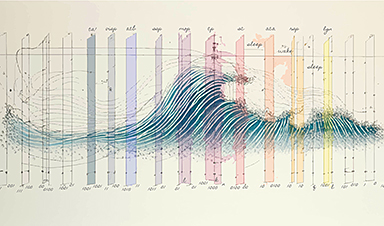
Small regions of the brain can take micro-naps while the rest of the brain is awake and vice versa
Sleep and wake: They're totally distinct states of being that define the boundaries of our daily lives. For years, scientists have measured the difference between these instinctual brain processes by observing brain waves, with [...]
Redefining Consciousness: Small Regions of the Brain Can Take Micro-Naps While the Rest of the Brain Is Awake
The study broadly reveals how fast brain waves, previously overlooked, establish fundamental patterns of sleep and wakefulness. Scientists have developed a new method to analyze sleep and wake states by detecting ultra-fast neuronal activity [...]
AI Reveals Health Secrets Through Facial Temperature Mapping
Researchers have found that different facial temperatures correlate with chronic illnesses like diabetes and high blood pressure, and these can be detected using AI with thermal cameras. They highlight the potential of this technology [...]
Breakthrough in aging research: Blocking IL-11 extends lifespan and improves health in mice
In a recent study published in the journal Nature, a team of researchers used murine models and various pharmacological and genetic approaches to examine whether pro-inflammatory signaling involving interleukin (IL)-11, which activates signaling molecules such [...]
Promise for a universal influenza vaccine: Scientists validate theory using 1918 flu virus
New research led by Oregon Health & Science University reveals a promising approach to developing a universal influenza vaccine—a so-called "one and done" vaccine that confers lifetime immunity against an evolving virus. The study, [...]
New Projects Aim To Pioneer the Future of Neuroscience
One study will investigate the alterations in brain activity at the cellular level caused by psilocybin, the psychoactive substance found in “magic mushrooms.” How do neurons respond to the effects of magic mushrooms? What [...]
Decoding the Decline: Scientific Insights Into Long COVID’s Retreat
Research indicates a significant reduction in long COVID risk, largely due to vaccination and the virus’s evolution. The study analyzes data from over 441,000 veterans, showing lower rates of long COVID among vaccinated individuals compared [...]
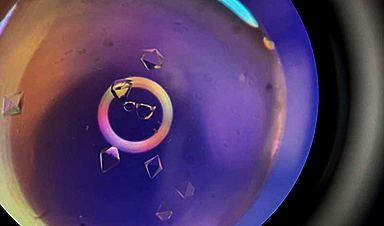
Silicon Transformed: A Breakthrough in Laser Nanofabrication
A new method enables precise nanofabrication inside silicon using spatial light modulation and laser pulses, creating advanced nanostructures for potential use in electronics and photonics. Silicon, the cornerstone of modern electronics, photovoltaics, and photonics, [...]
Caught in the actinium: New research could help design better cancer treatments
The element actinium was first discovered at the turn of the 20th century, but even now, nearly 125 years later, researchers still don't have a good grasp on the metal's chemistry. That's because actinium [...]
Innovative Light-Controlled Drugs Could Revolutionize Neuropathic Pain Treatment
A team of researchers from the Institute for Bioengineering of Catalonia (IBEC) has developed light-activated derivatives of the anti-epileptic drug carbamazepine to treat neuropathic pain. Light can be harnessed to target drugs to specific [...]
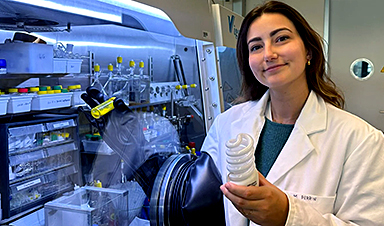
Green Gold: Turning E-Waste Into a Treasure Trove of Rare Earth Metals
Scientists are developing a process inspired by nature that efficiently recovers europium from old fluorescent lamps. The approach could lead to the long-awaited recycling of rare earth metals. A small molecule that naturally serves [...]
Cambridge Study: AI Chatbots Have an “Empathy Gap,” and It Could Be Dangerous
A new study suggests a framework for “Child Safe AI” in response to recent incidents showing that many children perceive chatbots as quasi-human and reliable. A study has indicated that AI chatbots often exhibit [...]
Nanoparticle-based delivery system could offer treatment for diabetics with rare insulin allergy
Up to 3% of people with diabetes have an allergic reaction to insulin. A team at Forschungszentrum Jülich has now studied a method that could be used to deliver the active substance into the [...]