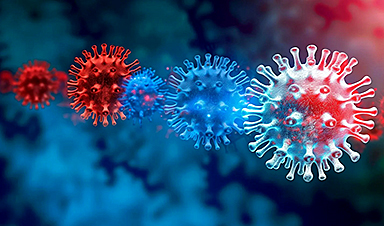
Evidence is mounting that Omicron’s new sister variant, known as BA.2, is more transmissible than the original strain but at this stage does not appear to be more vaccine-evasive.
The subvariant BA.2 is one of at least three sub-lineages of Omicron, the strain of COVID-19 first spotted in Africa in late November and now dominant around much of the world.
While rare in Australia and most other countries – the virus is found in about 2 per cent of local samples – BA.2 has started to gain a serious foothold in England, India and Denmark, where it has out-competed Omicron and now makes up most viruses sampled.
“That does seem to suggest there is an intrinsic transmissibility advantage,” said Dr Adam Wheatley, who heads a research team studying the immune response to COVID-19 at the University of Melbourne.
Instead, BA.2 is likely to slowly replace Omicron, much as a variant known as D614G quietly replaced the version of the virus that emerged from Wuhan in the middle of 2020.
“Nothing ominous has come out so far. There is no reason to panic,” said Professor Seshadri Vasan, who has been tracking COVID-19’s variants at the CSIRO.
Preliminary data released by Britain’s Health Security Agency earlier this week suggests a two-dose course of vaccine provides essentially no protection against catching either Omicron or BA.2
“The take-home message is: if you are not vaccinated, please go and get that first dose. And if you are double-vaccinated, please go and book a booster,” Professor Vasan said.
Just 34.6 per cent of Australians aged over 12 have had a booster, leaving much of the population vulnerable to Omicron and BA.2.
Evidence from a small number of Omicron infections tracked by British health authorities suggests BA.2’s “secondary attack rate” – the chance of an infected person passing the virus on to someone else in the household – is 13.4 per cent, compared with 10.3 per cent for Omicron.
Scientists are focusing on three main theories to explain Omicron’s emergence.
One possibility: an unknown group of people who have been harbouring an older version of the virus, even as Delta spread around the world. Omicron may have evolved there and then emerged.
Another option: COVID-19 has spilled back from humans into animals, where it has picked up new mutations before jumping back into humans as Omicron. There is good evidence now that a range of animals can be infected with COVID-19, including mink and deer. Denmark culled millions of mink after the animals came down with the virus; late last year US scientists discovered wild deer had become a huge reservoir of COVID-19.
But the most likely option, Dr Wheatley said, was Omicron emerged from a single unlucky individual. This person may have HIV or be being treated with drugs to suppress the immune system. Because their immune system was so weak, they could have been infected with COVID-19 for months.
“You have a situation where you have a virus in a person for a long time, you have an immune system that’s not functioning, and you can get lots of mutations in one person,” said Dr Wheatley.
News
The Silent Battle Within: How Your Organs Choose Between Mom and Dad’s Genes
Research reveals that selective expression of maternal or paternal X chromosomes varies by organ, driven by cellular competition. A new study published today (July 26) in Nature Genetics by the Lymphoid Development Group at the MRC [...]
Study identifies genes increasing risk of severe COVID-19
Whether or not a person becomes seriously ill with COVID-19 depends, among other things, on genetic factors. With this in mind, researchers from the University Hospital Bonn (UKB) and the University of Bonn, in [...]
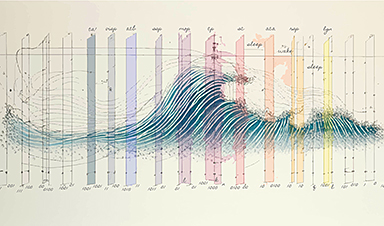
Small regions of the brain can take micro-naps while the rest of the brain is awake and vice versa
Sleep and wake: They're totally distinct states of being that define the boundaries of our daily lives. For years, scientists have measured the difference between these instinctual brain processes by observing brain waves, with [...]
Redefining Consciousness: Small Regions of the Brain Can Take Micro-Naps While the Rest of the Brain Is Awake
The study broadly reveals how fast brain waves, previously overlooked, establish fundamental patterns of sleep and wakefulness. Scientists have developed a new method to analyze sleep and wake states by detecting ultra-fast neuronal activity [...]
AI Reveals Health Secrets Through Facial Temperature Mapping
Researchers have found that different facial temperatures correlate with chronic illnesses like diabetes and high blood pressure, and these can be detected using AI with thermal cameras. They highlight the potential of this technology [...]
Breakthrough in aging research: Blocking IL-11 extends lifespan and improves health in mice
In a recent study published in the journal Nature, a team of researchers used murine models and various pharmacological and genetic approaches to examine whether pro-inflammatory signaling involving interleukin (IL)-11, which activates signaling molecules such [...]
Promise for a universal influenza vaccine: Scientists validate theory using 1918 flu virus
New research led by Oregon Health & Science University reveals a promising approach to developing a universal influenza vaccine—a so-called "one and done" vaccine that confers lifetime immunity against an evolving virus. The study, [...]
New Projects Aim To Pioneer the Future of Neuroscience
One study will investigate the alterations in brain activity at the cellular level caused by psilocybin, the psychoactive substance found in “magic mushrooms.” How do neurons respond to the effects of magic mushrooms? What [...]
Decoding the Decline: Scientific Insights Into Long COVID’s Retreat
Research indicates a significant reduction in long COVID risk, largely due to vaccination and the virus’s evolution. The study analyzes data from over 441,000 veterans, showing lower rates of long COVID among vaccinated individuals compared [...]
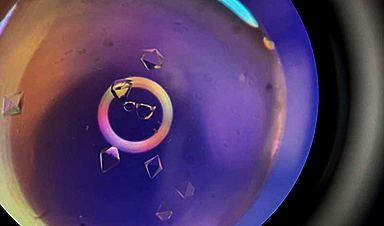
Silicon Transformed: A Breakthrough in Laser Nanofabrication
A new method enables precise nanofabrication inside silicon using spatial light modulation and laser pulses, creating advanced nanostructures for potential use in electronics and photonics. Silicon, the cornerstone of modern electronics, photovoltaics, and photonics, [...]
Caught in the actinium: New research could help design better cancer treatments
The element actinium was first discovered at the turn of the 20th century, but even now, nearly 125 years later, researchers still don't have a good grasp on the metal's chemistry. That's because actinium [...]
Innovative Light-Controlled Drugs Could Revolutionize Neuropathic Pain Treatment
A team of researchers from the Institute for Bioengineering of Catalonia (IBEC) has developed light-activated derivatives of the anti-epileptic drug carbamazepine to treat neuropathic pain. Light can be harnessed to target drugs to specific [...]
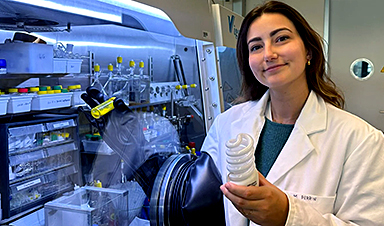
Green Gold: Turning E-Waste Into a Treasure Trove of Rare Earth Metals
Scientists are developing a process inspired by nature that efficiently recovers europium from old fluorescent lamps. The approach could lead to the long-awaited recycling of rare earth metals. A small molecule that naturally serves [...]
Cambridge Study: AI Chatbots Have an “Empathy Gap,” and It Could Be Dangerous
A new study suggests a framework for “Child Safe AI” in response to recent incidents showing that many children perceive chatbots as quasi-human and reliable. A study has indicated that AI chatbots often exhibit [...]
Nanoparticle-based delivery system could offer treatment for diabetics with rare insulin allergy
Up to 3% of people with diabetes have an allergic reaction to insulin. A team at Forschungszentrum Jülich has now studied a method that could be used to deliver the active substance into the [...]
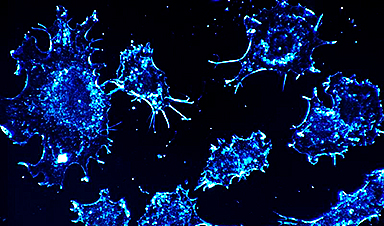
Nanorobot kills cancer cells in mice with hidden weapon
Researchers at Karolinska Institutet in Sweden have developed nanorobots that kill cancer cells in mice. The robot's weapon is hidden in a nanostructure and is exposed only in the tumor microenvironment, sparing healthy cells. [...]