When Srikanth Singamaneni and Guy Genin, both professors of mechanical engineering and materials science at the McKelvey School of Engineering at Washington University in St. Louis, established a new collaboration with researchers from the School of Medicine in late 2019, they didn’t know the landscape of infectious disease research was about to shift dramatically. In a conference room overlooking Forest Park on a beautiful fall day, the team had one goal in mind: tackle the biggest infectious disease problem facing the world right then.
“Greg Storch told us that one of the most important challenges facing the field of infectious disease is finding a way to figure out quickly if a patient has a bacterial infection and should get antibiotics or has a viral infection, for which antibiotics will not be effective.”
Storch, MD, the Ruth L. Siteman Professor of Pediatrics at the School of Medicine, was interested in diseases that affect most people regularly—colds, strep throat or the flu—but that weren’t getting as much research attention as rarer diseases. “Even with great advances that have been made in infectious disease diagnostics, there is still a niche for tests that are simple, rapid and sensitive,” Storch said. “It would be especially powerful if they could provide quantitative information. Tests with these characteristics could be employed in sophisticated laboratories or in the field.”
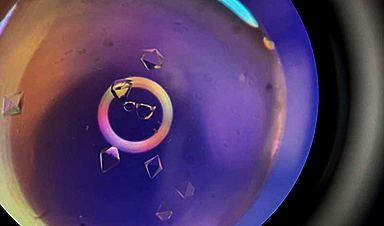
Drawing on his years of experience in developing nanomaterials for applications in biology and medicine, Singamaneni, the Lilyan & E. Lisle Hughes Professor, sought to overcome these limitations in point-of-care diagnostic tests. Singamaneni and his lab developed ultrabright fluorescent nanolabels called plasmonic-fluors, which could be quickly integrated into a common testing platform, the lateral flow assay (LFA).
Plasmon-enhanced LFAs (p-LFAs) improve inexpensive, readily available rapid tests to levels of sensitivity required by physicians for confidence in test results without the need for lab-based confirmation.
According to findings published Feb. 2 in Nature Biomedical Engineering, the team’s p-LFAs are 1,000 times more sensitive than conventional LFAs, which show results via a visual color and fluorescence signal on the strip. When analyzed using a fluorescence scanner, p-LFAs are also substantially faster than gold-standard lab tests, returning results in only 20 minutes instead of several hours, with comparable or improved sensitivity. The p-LFAs can detect and quantify concentrations of proteins, enabling them to detect bacterial and viral infections as well as markers of inflammation that point to other diseases.
“Our p-LFAs can pick up even very small concentrations of antibodies and antigens, typical markers of infection, and give clinicians clear, quick results without the need for specialized equipment. For quantitative testing beyond the initial screening, the same LFA strip can be scanned with a fluorescence reader, enabling rapid and ultrasensitive colorimetric and fluorometric detection of disease markers with only one test.”
“It’s like turning up the volume on standard color-changing test strips. Instead of getting a faint line indicating only a positive or negative result, the new p-LFAs give clearer results with fewer particles, enabling one to move from simply ‘yes or no?’ to exactly ‘how much?’ with the aid of an inexpensive, portable scanner,” said Jeremiah Morrissey, a research professor in anesthesiology in the Division of Clinical and Translational Research at the School of Medicine. Morrissey is a co-author of the new study and a long-term collaborator with the Singamaneni lab.
This improved testing capability has obvious benefits for a population now all too familiar with the need for quick and reliable test results and the risk of false negatives.
“When we took on this problem in 2019, we thought our biggest challenge would be getting an adequate number of samples from sick people,” Genin recalled. “Where on Earth could we find a massive set of samples from patients whose symptoms were carefully documented and whose diagnosis was verified by slow and expensive PCR tests?” In a matter of months, COVID-19 would erase that obstacle while introducing a whole host of new challenges and opportunities.
“The pandemic was a big shift for us, like it was for everyone,” said first author Rohit Gupta, who worked on the p-LFA study as a graduate student in Singamaneni’s lab and is now a senior scientist at Pfizer. “We had to move away from our original focus on distinguishing viruses from bacteria, but it turned out to be an opportunity to do practical science with real stakes. We were working with epidemiologists to get samples for testing, with diagnosticians to compare our test to what was available, and with clinicians to gain insights into the real needs for patient care.”
Input from the entire collaboration helped Gupta and Singamaneni refine the design of the p-LFAs, which ultimately achieved 95% clinical sensitivity and 100% specificity for SARS-CoV-2 antibodies and antigens. Genin described the results as stunning.
“We didn’t know it was going to work so well,” he said. “We knew it would be good, but we didn’t know this $1 test with a $300 readout device would be so much better—10 times better—than state of the art that we all used during the COVID pandemic.”
Now that they’ve proven p-LFAs can outperform standard lab tests in sensitivity, speed, convenience and cost for one disease, the team is looking to develop new applications for the technology, including returning to their original goal of identifying bacterial versus viral infections and getting their diagnostic tool into the hands of physicians around the world.
The p-LFA technology has been licensed to Auragent Bioscience LLC by Washington University’s Office of Technology Management. Singamaneni and Morrissey are among the co-founders of Auragent, a WashU startup.
“We expect to have p-LFAs commercially available in the next one to two years,” Singamaneni said. “Right now, we’re working on improving our portable scanner technology, which adds a more sensitive, fluorescent reading capability to the test strips in addition to the color change that can be seen with the naked eye. We think we can get that cost down to a point where it’s accessible to rural clinics in the U.S. and abroad, which was one of our original goals.”
“We’re also excited about the potential to detect many more diseases than COVID, possibly using a skin patch that can take a painless sample,” Singamaneni added. “This technology has the potential to detect any number of diseases, ranging from STIs to respiratory infections and more, as well as cytokines indicative of inflammation seen in conditions such as rheumatoid arthritis and sepsis.”
News
The Silent Battle Within: How Your Organs Choose Between Mom and Dad’s Genes
Research reveals that selective expression of maternal or paternal X chromosomes varies by organ, driven by cellular competition. A new study published today (July 26) in Nature Genetics by the Lymphoid Development Group at the MRC [...]
Study identifies genes increasing risk of severe COVID-19
Whether or not a person becomes seriously ill with COVID-19 depends, among other things, on genetic factors. With this in mind, researchers from the University Hospital Bonn (UKB) and the University of Bonn, in [...]
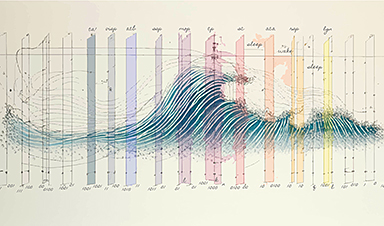
Small regions of the brain can take micro-naps while the rest of the brain is awake and vice versa
Sleep and wake: They're totally distinct states of being that define the boundaries of our daily lives. For years, scientists have measured the difference between these instinctual brain processes by observing brain waves, with [...]
Redefining Consciousness: Small Regions of the Brain Can Take Micro-Naps While the Rest of the Brain Is Awake
The study broadly reveals how fast brain waves, previously overlooked, establish fundamental patterns of sleep and wakefulness. Scientists have developed a new method to analyze sleep and wake states by detecting ultra-fast neuronal activity [...]
AI Reveals Health Secrets Through Facial Temperature Mapping
Researchers have found that different facial temperatures correlate with chronic illnesses like diabetes and high blood pressure, and these can be detected using AI with thermal cameras. They highlight the potential of this technology [...]
Breakthrough in aging research: Blocking IL-11 extends lifespan and improves health in mice
In a recent study published in the journal Nature, a team of researchers used murine models and various pharmacological and genetic approaches to examine whether pro-inflammatory signaling involving interleukin (IL)-11, which activates signaling molecules such [...]
Promise for a universal influenza vaccine: Scientists validate theory using 1918 flu virus
New research led by Oregon Health & Science University reveals a promising approach to developing a universal influenza vaccine—a so-called "one and done" vaccine that confers lifetime immunity against an evolving virus. The study, [...]
New Projects Aim To Pioneer the Future of Neuroscience
One study will investigate the alterations in brain activity at the cellular level caused by psilocybin, the psychoactive substance found in “magic mushrooms.” How do neurons respond to the effects of magic mushrooms? What [...]
Decoding the Decline: Scientific Insights Into Long COVID’s Retreat
Research indicates a significant reduction in long COVID risk, largely due to vaccination and the virus’s evolution. The study analyzes data from over 441,000 veterans, showing lower rates of long COVID among vaccinated individuals compared [...]
Silicon Transformed: A Breakthrough in Laser Nanofabrication
A new method enables precise nanofabrication inside silicon using spatial light modulation and laser pulses, creating advanced nanostructures for potential use in electronics and photonics. Silicon, the cornerstone of modern electronics, photovoltaics, and photonics, [...]
Caught in the actinium: New research could help design better cancer treatments
The element actinium was first discovered at the turn of the 20th century, but even now, nearly 125 years later, researchers still don't have a good grasp on the metal's chemistry. That's because actinium [...]
Innovative Light-Controlled Drugs Could Revolutionize Neuropathic Pain Treatment
A team of researchers from the Institute for Bioengineering of Catalonia (IBEC) has developed light-activated derivatives of the anti-epileptic drug carbamazepine to treat neuropathic pain. Light can be harnessed to target drugs to specific [...]
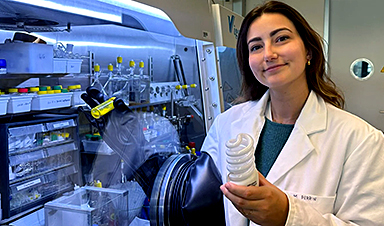
Green Gold: Turning E-Waste Into a Treasure Trove of Rare Earth Metals
Scientists are developing a process inspired by nature that efficiently recovers europium from old fluorescent lamps. The approach could lead to the long-awaited recycling of rare earth metals. A small molecule that naturally serves [...]
Cambridge Study: AI Chatbots Have an “Empathy Gap,” and It Could Be Dangerous
A new study suggests a framework for “Child Safe AI” in response to recent incidents showing that many children perceive chatbots as quasi-human and reliable. A study has indicated that AI chatbots often exhibit [...]
Nanoparticle-based delivery system could offer treatment for diabetics with rare insulin allergy
Up to 3% of people with diabetes have an allergic reaction to insulin. A team at Forschungszentrum Jülich has now studied a method that could be used to deliver the active substance into the [...]
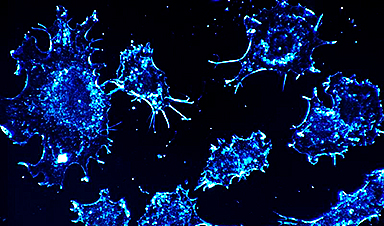
Nanorobot kills cancer cells in mice with hidden weapon
Researchers at Karolinska Institutet in Sweden have developed nanorobots that kill cancer cells in mice. The robot's weapon is hidden in a nanostructure and is exposed only in the tumor microenvironment, sparing healthy cells. [...]