Although combining radiation therapy (RT) with immune checkpoint blockade (ICB) could activate an in situ vaccine effect, RT limits the tumor antigen presentation and cannot overcome suppressive mechanisms in the tumor microenvironment (TME), limiting the vaccine effect.
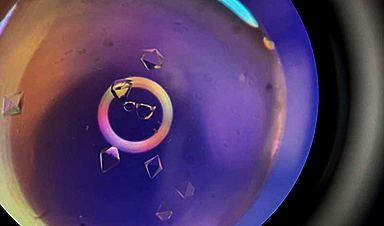
An article published in the journal Nature Communications presented a solution to overcome the above challenges by developing PIC multifunctional nanoparticles based on poly-(L-lysine) (PLL), CpG oligodeoxynucleotide (CpG), and iron oxide nanoparticles (ION). The designed nanoparticles served as radiation sensitizers, improved the tumor antigen presentation, increased the M1:M2 ratio of tumor-associated macrophages, and enhanced the stimulation of a type I interferon response combined with RT.
The therapy using the combination of RT, PIC nanoparticles, and ICB in immunologically “cold” murine tumor models improved the tumor response, increased the survival rate, and activated the tumor-specific immune memory. Utilizing the designed PIC nanoparticles in RT evoked the in situ vaccine effect, potentiated adaptive anti-tumor immunity, and augmented the response to ICB and other potential immunotherapies.
Role of Nanoparticles in Cancer Immunotherapy
Despite the success of cancer immunotherapy, patients with immunologically “cold” tumors are less likely to respond to ICB therapy. The “cold” tumors are characterized by limited immune cell infiltration and low neoantigen load. The in situ cancer vaccination converts a patient’s tumor into a nidus to present tumor-specific antigens and to stimulate and diversify anti-tumor T cell response. Thus, improving the response rates of immunologically “cold” tumors.
At least half of cancer patients receive RT at some point in their cancer treatment which helps in activating the in situ vaccine response. RT stimulates the immunogenic cell apoptosis, increases tumor infiltration by immune cells, and enhances the immune-mediated killing of tumor cells. Although RT may induce many favorable effects in the tumor microenvironment (TME), it may also lead to detrimental effects on cells due to a lack of specificity.
Due to the development of nanotechnology, nanomaterials with heavy metals showed promising radio-sensitization to enhance the favorable RT outcomes, such as gold and silver nanoparticles, which can efficiently absorb, scatter, emit radiation energy, and are easily eliminated by metabolism. Recently, cancer immunotherapy has emerged as a promising treatment, and immune checkpoint regulation has the potential property to improve clinical outcomes in cancer immunotherapy.
Multifunctional Nanoparticles to Potentiate the In Situ Vaccination Effect
The cancer immunotherapy resistant “cold” tumors are characterized by low tumor neoantigen load, few tumor-infiltrating effector T cells, and activation of immune suppressive mechanisms in TME. Previously conducted clinical studies confirmed the safe combination of RT and ICB in improving response and survival rate, particularly in patients with “cold” tumors.
Besides the above advantages, RT was also reported to cause detrimental local effects on the TME. To increase the capacity of RT in eliciting in situ vaccination, the combination of RT with the therapeutic agent was hypothesized to augment the effect of RT in activating T-cell immunity.
In the present work, PIC nanoparticles were designed to improve the in situ vaccine effect of RT, facilitate anticancer response against “cold” tumors, and increase their response to ICBs. The results suggested that this approach could offer an effective strategy that permits the use of off-the-shelf treatment in realizing in situ vaccine effect. Here a patient’s tumor is transformed into nidus to present tumor-specific antigens, stimulating and diversifying the anti-tumor T cell response against the patient’s cancer cells.
Additionally, combining anti-CTLA-4 with PIC nanoparticles and RT in situ vaccination showed greater tumor response, improving the survival rate and tumor-specific immune memory compared to RT or PIC nanoparticles or combined treatment. Moreover, the mouse model treated with PIC nanoparticles + RT or PIC nanoparticles + RT + anti-CTLA-4 did not show any hepatic, gastrointestinal, renal, or autoimmune toxicities, confirming the biosafety of the proposed strategy.
Conclusion
To summarize, the present work demonstrated that the designed PIC nanoparticles had the advantages of reproducibility and scalability. Following RT, the nanoparticles modulated the tumor-immune microenvironment, favoring the activation of an in situ vaccine effect.
Immunotherapies and ICBs are extensively used to treat cancer patients. However, the limiting response of “cold” cancers to these therapies was an issue of concern. The multifunctional PIC nanoparticles resolved the above issue by potentiating the vaccination effect and augmenting the response rate of “cold” cancers to ICBs.
Thus, the results confirmed the promising application of PIC nanoparticles in combination with ICB and RT and its translation to the preclinical and early phases of clinical trials in treating metastatic cancers.
News
The Silent Battle Within: How Your Organs Choose Between Mom and Dad’s Genes
Research reveals that selective expression of maternal or paternal X chromosomes varies by organ, driven by cellular competition. A new study published today (July 26) in Nature Genetics by the Lymphoid Development Group at the MRC [...]
Study identifies genes increasing risk of severe COVID-19
Whether or not a person becomes seriously ill with COVID-19 depends, among other things, on genetic factors. With this in mind, researchers from the University Hospital Bonn (UKB) and the University of Bonn, in [...]
Small regions of the brain can take micro-naps while the rest of the brain is awake and vice versa
Sleep and wake: They're totally distinct states of being that define the boundaries of our daily lives. For years, scientists have measured the difference between these instinctual brain processes by observing brain waves, with [...]
Redefining Consciousness: Small Regions of the Brain Can Take Micro-Naps While the Rest of the Brain Is Awake
The study broadly reveals how fast brain waves, previously overlooked, establish fundamental patterns of sleep and wakefulness. Scientists have developed a new method to analyze sleep and wake states by detecting ultra-fast neuronal activity [...]
AI Reveals Health Secrets Through Facial Temperature Mapping
Researchers have found that different facial temperatures correlate with chronic illnesses like diabetes and high blood pressure, and these can be detected using AI with thermal cameras. They highlight the potential of this technology [...]
Breakthrough in aging research: Blocking IL-11 extends lifespan and improves health in mice
In a recent study published in the journal Nature, a team of researchers used murine models and various pharmacological and genetic approaches to examine whether pro-inflammatory signaling involving interleukin (IL)-11, which activates signaling molecules such [...]
Promise for a universal influenza vaccine: Scientists validate theory using 1918 flu virus
New research led by Oregon Health & Science University reveals a promising approach to developing a universal influenza vaccine—a so-called "one and done" vaccine that confers lifetime immunity against an evolving virus. The study, [...]
New Projects Aim To Pioneer the Future of Neuroscience
One study will investigate the alterations in brain activity at the cellular level caused by psilocybin, the psychoactive substance found in “magic mushrooms.” How do neurons respond to the effects of magic mushrooms? What [...]
Decoding the Decline: Scientific Insights Into Long COVID’s Retreat
Research indicates a significant reduction in long COVID risk, largely due to vaccination and the virus’s evolution. The study analyzes data from over 441,000 veterans, showing lower rates of long COVID among vaccinated individuals compared [...]
Silicon Transformed: A Breakthrough in Laser Nanofabrication
A new method enables precise nanofabrication inside silicon using spatial light modulation and laser pulses, creating advanced nanostructures for potential use in electronics and photonics. Silicon, the cornerstone of modern electronics, photovoltaics, and photonics, [...]
Caught in the actinium: New research could help design better cancer treatments
The element actinium was first discovered at the turn of the 20th century, but even now, nearly 125 years later, researchers still don't have a good grasp on the metal's chemistry. That's because actinium [...]
Innovative Light-Controlled Drugs Could Revolutionize Neuropathic Pain Treatment
A team of researchers from the Institute for Bioengineering of Catalonia (IBEC) has developed light-activated derivatives of the anti-epileptic drug carbamazepine to treat neuropathic pain. Light can be harnessed to target drugs to specific [...]
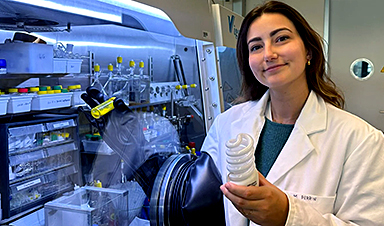
Green Gold: Turning E-Waste Into a Treasure Trove of Rare Earth Metals
Scientists are developing a process inspired by nature that efficiently recovers europium from old fluorescent lamps. The approach could lead to the long-awaited recycling of rare earth metals. A small molecule that naturally serves [...]
Cambridge Study: AI Chatbots Have an “Empathy Gap,” and It Could Be Dangerous
A new study suggests a framework for “Child Safe AI” in response to recent incidents showing that many children perceive chatbots as quasi-human and reliable. A study has indicated that AI chatbots often exhibit [...]
Nanoparticle-based delivery system could offer treatment for diabetics with rare insulin allergy
Up to 3% of people with diabetes have an allergic reaction to insulin. A team at Forschungszentrum Jülich has now studied a method that could be used to deliver the active substance into the [...]
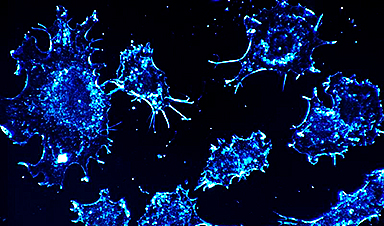
Nanorobot kills cancer cells in mice with hidden weapon
Researchers at Karolinska Institutet in Sweden have developed nanorobots that kill cancer cells in mice. The robot's weapon is hidden in a nanostructure and is exposed only in the tumor microenvironment, sparing healthy cells. [...]