At Cambridge University’s MRC Mitochondrial Biology Unit, Michal Minczuk is one of a growing number of scientists around the world aiming to find new ways of improving mitochondrial health. This line of research could help provide much-needed treatments for people with long Covid, as well as revolutionising our understanding of everything from neurodegenerative illnesses such as Parkinson’s disease to the ageing process.
Mitochondria, tiny tube-shaped structures that are found in their hundreds, sometimes thousands, in nearly all of our cells, are best known as the body’s power plants, continuously converting the food we eat into ATP, a complex chemical that acts as a form of energy currency for cells. Without ATP, every one of our cells, from the brain to the muscles, would lack the fuel they need to keep churning away, and our organs would swiftly grind to a halt.
But while mitochondria are often typecast as energy factories, scientists have repeatedly discovered that they do far more than simply generate ATP. For one thing, they can help keep us warm when we are cold via an alternative form of heat generation to shivering, and studies have suggested that mitochondria in the eye even play a role in focusing light on to the retina, helping us perceive our environment.
In fact, the more we look, the more we find that they contribute to the many building blocks of life that keep us healthy, from synthesising the protein haemoglobin, which transports oxygen in the bloodstream, to storing calcium, and even the immune system response. While mitochondria sustain our cells, they also play a critical role in the natural process of cell death that occurs over and over again throughout our lives, identifying old and damaged cells which must be cleared away and destroyed.
Put simply they are vital to our survival, but like much of the body’s innate machinery, we only notice them when they start to go wrong. “Mitochondria are involved in many processes so when they don’t function well, this can precipitate different types of dysfunction in the human body leading to disease,” says Minczuk.
One of the unique complexities of mitochondria is that they have their own DNA, separate from the DNA stored in the nuclei of our cells, which comes from both parents. Mitochondrial DNA (mtDNA) is passed down from the mother only, and consists of fewer than 17,000 base pairs, compared with 3.3bn in the nucleus. But it still encodes specific instructions for a number of proteins, and over the past decade, scientists have found that mutations in mtDNA that prevent mitochondria from functioning normally can affect our health, contributing to a variety of chronic illnesses.
The most drastic cases are so-called mitochondrial diseases where mutations in mtDNA are acquired genetically. They affect around one in 4,300 people, and the consequences are grave. The life expectancy for most patients is between 10 and 35 years, with most dying from general body wasting owing to brain or muscle damage, or impairments to organs such as the heart and kidneys. But studies have also shown that mutations can accumulate in mtDNA as we age, and Minczuk’s research group at the University of Cambridge MRC mitochondrial biology unit is particularly interested in the role this might play in Parkinson’s.
It is thought that some Parkinson’s patients have genetic mutations that prevent damaged mitochondria being eliminated and replaced with healthy versions – a process called autophagy. As a result, the existing mitochondria in the body accrue more and more mutations, with damaging consequences for cells such as neurons, which rely heavily on the energy they supply.
But the rise of new gene-editing techniques may offer new treatment solutions in the years to come, initially for mitochondrial diseases but possibly for other illnesses too. This has been a challenge because Crispr technology – which uses a piece of RNA to guide an enzyme to a specific DNA location where it cuts out a mutation – cannot be used to tweak mitochondria, as it is not possible to deliver RNA into mtDNA.
However over the past few years, scientists including Minczuk have designed enzymes that can achieve the same effect as Crispr without requiring RNA. While studies are still being conducted on rodents, this offers enormous future potential.
“We’re slowly gathering the tools to be able to modify the mitochondrial genome in animal cells,” Minczuk says. “Right now we could eliminate existing mutations, changing the genetic make-up of mitochondria, but we also want to be able to trigger new mutations. This would allow us to study Parkinson’s in far more detail. We could take a healthy mouse, for example, and introduce mutations seen in Parkinson’s patients, and see what happens. Would that trigger the onset of symptoms?”
Treating long Covid
At Oxford University, cardiologist Betty Raman is currently in the middle of running a clinical trial to see whether an amino acid cocktail known as AXA1125, produced by Massachusetts-based biotech Axcella Therapeutics, can help long Covid patients where fatigue is by far the dominant symptom.
“The drug is a powdered drink, consumed three times a day along with meals, and we’re hoping that it will help people with their energy levels and fatigue,” she says. “The idea is that it can give the mitochondria additional fuel to produce energy, and help repair damaged mitochondria. Hopefully, by the end of July, we should have some top line results to report.”
The idea that mitochondria may be involved in the ailments of some of those with long Covid arises from research conducted by Raman and others on patients who find themselves chronically exhausted by exercise following Covid-19, despite showing no obvious heart or lung abnormalities. This symptom is often referred to as post-exertional malaise (PEM), and is also experienced by people with genetic mitochondrial diseases.
In long Covid patients with PEM, Raman has found that their muscles struggle to extract oxygen from the blood as efficiently as might be expected. After coming across research that showed that mitochondria in white blood cells were not as efficient in generating ATP in patients recovering from Covid-19, she concluded that this might be the root cause.
But why do the mitochondria of these patients become sluggish in generating ATP? David Systrom, a pulmonary and critical care doctor at Brigham & Women’s Hospital, Boston, believes he has found answers through studying patients with ME/CFS, an illness that in many cases is precipitated by viral infections such as Epstein-Barr and bears many similarities to long Covid.
When Systrom studied the mitochondrial DNA of these patients it appeared to be normal, but after taking a deep look and conducting muscle biopsies, he identified abnormalities at the electron level, deep within the mitochondria.
“In both ME/CFS and long Covid it’s most likely that these are acquired forms of mitochondrial dysfunction, perhaps related to the initial infection itself or an autoimmune response to a virus or both,” Systrom says. “This impedes the mitochondrial machinery, but doesn’t affect the DNA itself, and it means the mitochondria then fail to generate appropriate amounts of ATP to serve the needs of the muscles.”
Systrom is now running his own clinical trial in both ME/CFS and long Covid patients, in partnership with Japanese drug company Astellas, which has developed a drug that aims to restore normal mitochondrial metabolism.
Both Raman and Systrom agree that mitochondrial dysfunction is only likely to be a factor in a subset of long Covid and ME/CFS patients. However, because mitochondria are so ubiquitous throughout the body, damage inflicted to these structures across different organ types could contribute to the wide range of different symptoms that patients tend to report.
A common ailment reported by people with long Covid and ME/CFS is dysautonomia, a peculiar condition that causes a rapid increase in heartbeat and lightheadedness when patients attempt any form of activity. Raman says that this is often caused by damage to small sensory nerves in the skin, something that has been associated with mitochondrial dysfunction.
“There is a theory that the mitochondrial problem may come first,” she says. “And because nerves are high energy tissues, they are particularly dependent on normal mitochondrial function and ATP production.”…….
News
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
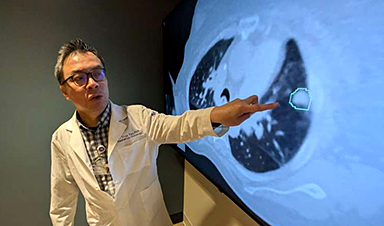
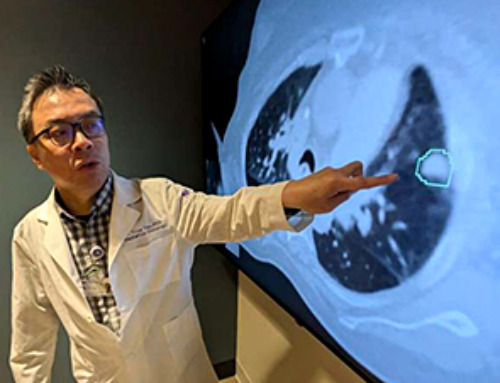
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]