The Linseman Laboratory is studying the long-term brain health effects of COVID-19 in individuals with and without traumatic brain injury (TBI). Preliminary data suggest that those with a history of both COVID-19 and TBI experience more severe long COVID symptoms. The study is also examining blood biomarkers to understand age-related differences in long COVID and explore potential treatments targeting neuroinflammatory pathways.
In January 2021, Ron Miller’s life was upended. The then-39-year-old, who described his health at the time as perfectly fine, contracted COVID-19. Two years later, he’s unable to work as he still suffers from extreme fatigue and brain fog—a byproduct of his battle with long COVID.
Ron’s not alone. In fact, he’s among the nearly 20% of people who’ve experienced lingering COVID-19 symptoms.
“It never really went away,” he says.
Ron, whose name has been changed for this story, is part of the Linseman Laboratory’s study on the long-term brain health effects of COVID-19 in people with and without traumatic brain injury (TBI).
The lab, which is run by University of Denver College of Natural Sciences and Mathematics professor Dan Linseman, is part of the Knoebel Institute for Healthy Aging. The lab’s work focuses on neuroinflammation, neurodegeneration, neurotrauma and now long-neurological COVID.
Traumatic brain injury (TBI) is a form of brain damage resulting from a sudden external force or impact that disrupts the normal function of the brain. It can be caused by events such as falls, car accidents, sports injuries, or violence, and ranges in severity from mild concussions to severe brain damage. TBI may lead to temporary or permanent cognitive, physical, and emotional impairments, with symptoms including headaches, memory loss, difficulty concentrating, mood swings, and altered speech or motor functions. Treatment and recovery depend on the severity of the injury and may involve medical intervention, rehabilitation, and ongoing support.
Allison Grossberg, a fourth-year doctoral student in the cellular and molecular biology program, is leading the study, which began in 2022 and partners with National Jewish Health and Resilience Code. Grossberg and Linseman wanted to know whether individuals with a history of both brain trauma and COVID-19 have worsened long-term neurological and psychological symptoms, increased inflammation, or an increased risk of neurodegenerative disease and/or auto-immunity.
“Certain infections like COVID-19 and Lyme disease can lead to inflammation in the brain—so why should they be any different?” Grossberg says.
So far, the Linseman Lab has preliminary data for 48 of the study’s participants, 28 of whom, like Ron, had COVID-19 and one or more TBIs; 11 had only a TBI; and five had only COVID. And four participants—the control group—had no history of COVID or TBI.
The study collects its data through a yearly visit in which participants complete a cognitive assessment and a detailed questionnaire and have blood drawn.
Linseman and Grossberg say it’s possible the findings may change over the five-year study as more participants are recruited. But as of now, the preliminary data is clear: Those with a history of COVID-19 and TBI reported more severe long COVID symptoms, a higher symptom burden, and more frequent symptoms.
For many of the study’s participants who have had a concussion, including Ron, it’s been decades since their injury.
“Concussions you get when you are young can cause persistent underlying damage, and some of that damage is likely persistent neuroinflammation,” Linseman says. “For example, we found that people who have Lyme disease have a certain cadre of neurological symptoms, but if they have a history of concussions, those symptoms are much worse. I think it’s similar with COVID. These are all neurotropic, so they get into the brain. They cause inflammation. If they do that on a background of sustained persistent neuroinflammation like a history of head injury, it basically becomes a cumulative effect on the brain.”
The study participants ranged in age from 18-83. Everyone who reported contracting COVID-19 had mild to moderate symptoms. Nasal congestion was the most reported, and chest pain and tightness were the most severe.
Those who reported having COVID-19 and TBI reported worse depressive symptoms, worse functional outcomes, and increased fatigue.
The study isn’t only recording information through a unique detailed questionnaire. Grossberg and Linseman are also examining biomarkers from the blood samples of each participant. Every cell in the body secretes lipid vesicles, Grossberg says, which are used to communicate with other cells in the body.
“They’re tagged with little markers that are specific to each cell type that releases them,” Grossberg says. “Inside these little packages are tons of important signaling molecules that help us understand what’s going on in someone’s brain as opposed to just what’s happening in the bloodstream.”
Then researchers can take the vesicles, or exosomes, from each patient and incubate them with cells grown in the lab.
“We expect that the exosomes from participants with history of COVID and TBI carry cargo that might cause an inflammatory response in the cell that is worse compared to exosomes from healthy control participants,” Grossberg says. “We expect it to look similar to the inflammatory response in cells exposed directly to a bacterial endotoxin, a lipopolysaccharide, which is known to cause inflammation,” Grossberg says.
According to the preliminary data, exosomes from those who had a combined history of COVID-19 and TBI caused inflammation in the lab-grown astrocytes.
What’s more, Linseman says, is the potential link between age and long COVID. When the study began, they anticipated that older people with a history of concussions would report the worst long COVID symptoms. So far in their findings, the opposite is true.
“That’s leading me into supporting the theory with the immune system and neuroinflammation that’s contributing to the symptomology,” Linseman says. “The biggest difference between older and younger people is that younger people have a more robust immune system.”
If their hypothesis is correct, and there’s a neuroinflammatory pathway that’s upended by COVID and TBI, researchers can start to explore potential treatments, like one that inhibits the inflammatory pathway.
While that discovery may be years in the making, the Linseman Lab’s study is making strides in the right direction.
For Ron, a DU graduate who was a partner in a risk management consulting firm, participating in this study means something—a tangible way to make an impact.
“If it could be helpful to society overall, not necessarily just me, it would be nice. Who knows if it will keep others from getting it in the future,” Ron says. “I have a lot of time on my hands, might as well use it to contribute some good.”
News
Team finds flawed data in recent study relevant to coronavirus antiviral development
The COVID pandemic illustrated how urgently we need antiviral medications capable of treating coronavirus infections. To aid this effort, researchers quickly homed in on part of SARS-CoV-2's molecular structure known as the NiRAN domain—an [...]
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
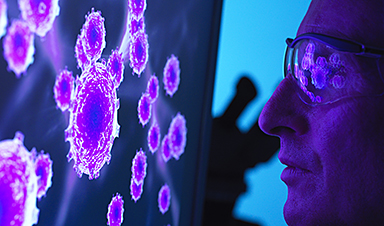
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
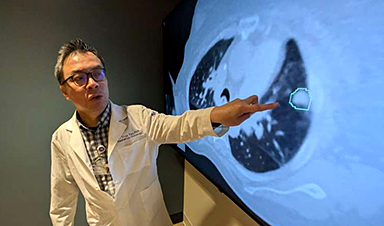
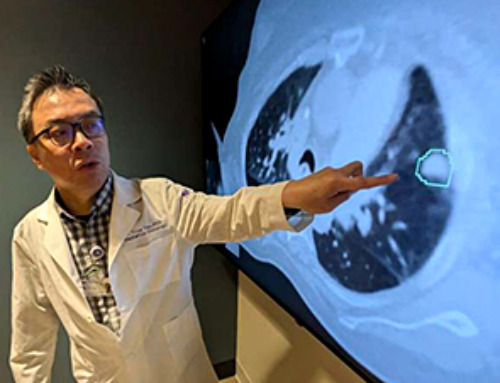
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
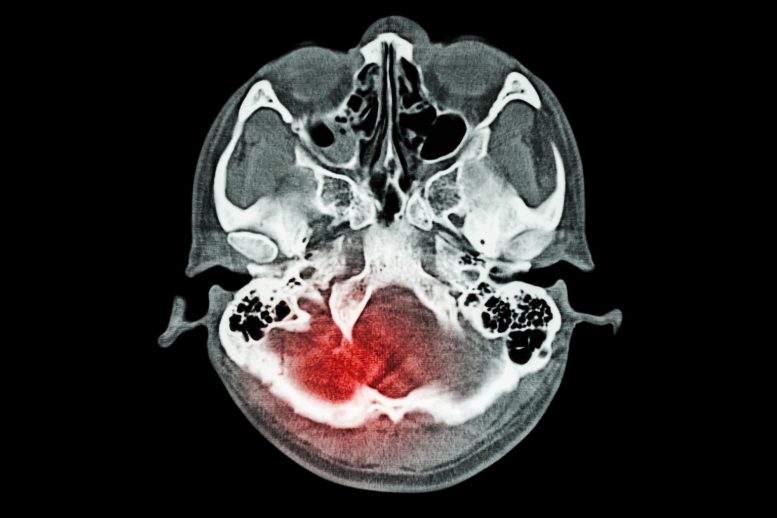
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]