When we breathe, the SARS-CoV-2 virus enters the body through the cells of the upper respiratory tract. Sensing an invader, the epithelial cells, which are the first line of defense, mount an immediate and broad “innate” defense and trigger an alarm.
The findings, by Dr. Gaetano Gargiulo, head of the “Molecular Oncology” lab, are reported in Science Advances.
This tool was originally developed in the Gargiulo lab to study cancer. But during the pandemic, the scientists decided to trial it in virus-infected cells. “Our team decided to create this tool to understand and fight viral infections in the spirit of doing our part during this pandemic,” says Gargiulo, senior author of the study. “It may be possible to rapidly address emerging pandemics in the future by tailoring our tool to recognize novel viral strains.”
Tracking the cell’s immune responses in real time
The tool is called “synthetic locus control region” (sLCR) and it consists of a lab-generated segment of DNA that switches a fluorescent protein on or off depending on whether the cell is mounting an immune response. During an innate immune response, the sLCR is turned on and it makes a protein that glows red when observed under a fluorescence microscope, telling scientists that the cell is aware of being infected and also how strongly it is fighting back.
The scientists constructed an sLCR containing several unique DNA sequences which they had predicted would be active during a SARS-CoV-2 infection based on other studies. They inserted the sLCRs into epithelial cells grown in a petri dish, which could then infected with the SARS-CoV-2 virus. The cells glowed red once the innate immunity was activated by the infection or surrogate biochemical cues, and they were visualized using fluorescence microscopy.
“The most exciting moment was when we saw that the infection with different strains of the live virus actually triggers the color coding,” says Ben Jiang, a graduate student at the Gargiulo lab and co-first author of the study. Experiments with the live viral particles were possible thanks to the inter-Helmholtz collaboration between the Gargiulo lab and the group led by Luka Cicin-Sain at the Helmholtz-Zentrum für Infektionsforschung (HZI) in Braunschweig.
Finding new treatments for viral diseases
Such a simple read out enabled the scientists to look for drugs that inhibited or enhanced cells’ responses to the virus. They found that cells treated with some rheumatoid arthritis drugs did not glow red, suggesting the drug blocked the immune response. When the cells were treated with certain chemotherapy drugs, the cells glowed more intensely, suggesting the drug enhanced the immune response.
The opposing effects may prove useful at different stages of COVID-19. At the start, a drug that provokes a strong immune response could help battle the virus. But later on in the disease, a prolonged response could worsen the pathology. “With a tool like this, one can identify compounds to strengthen or weaken the epithelial immune response, both of which can be useful depending on the disease stage and symptoms,” Jiang says.
In particular, the discovery that DNA damaging agents can enhance the alert signal from epithelial cells supports low-dose radiotherapy as a potential treatment for viral infections including COVID-19. This was tested during the pandemic, but needs precise dosage and timing, says Gargiulo.
Though this study was done in cell cultures, the drugs identified have been studied in clinical trials for COVID-19 by other groups. Hence, this tool could be used to screen drugs in bulk to find novel combinations and drugs that can be further trialed to see if they are effective in people. Moreover, “the technology could be easily applied to more sophisticated disease models, such as organoids or mice,” says the other co-first author Matthias Schmitt.
“The same approach can be readily re-purposed to target other viral infections, such as the emerging threat of Dengue and Zika viruses,” says Gargiulo “and the technology is accessible to labs around the world to find drugs to combat emerging infectious diseases timely.”
News
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
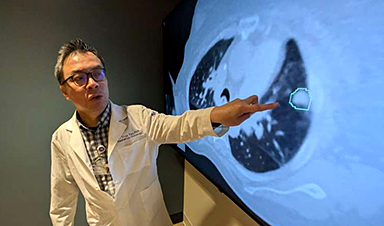
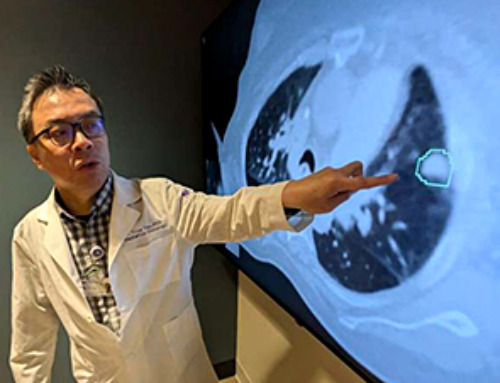
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
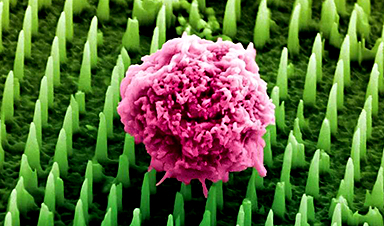
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]