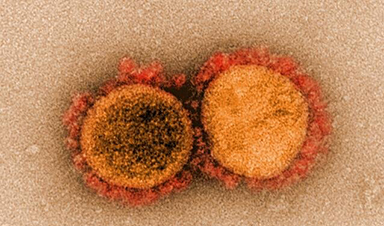
Scientists at The University of Texas MD Anderson Cancer Center and Northwestern Medicine have identified natural extracellular vesicles containing the ACE2 protein (evACE2) in the blood of COVID-19 patients that can block infection from broad strains of SARS-CoV-2 virus in preclinical studies. The study was published today in Nature Communications.
The study is the first to show evACE2 are capable of fighting the new SARS-CoV-2 variants with an equal or better efficacy than blocking the original strain. The researchers found that evACE2 exist in human blood as a natural anti-viral response. The more severe, the higher the levels of evACE2 detected in the patient’s blood.
“Whenever a new mutant strain of SARS-CoV-2 surges, the original vaccine and therapeutic antibodies may lose power against alpha, beta, delta and the most recent, omicron,” said co-senior author Huiping Liu, M.D., Ph.D., associate professor of pharmacology and medicine at Northwestern University Feinberg School of Medicine. “However, the beauty of evACE2 is its superpower in blocking broad strains of coronaviruses, including current SARS-CoV-2 and even future SARS coronaviruses from infecting humans. Our mouse studies demonstrate the therapeutic potential of evACE2 in preventing or blocking SARS-CoV-2 infection when it is delivered to the airway via droplets.”
The evACE2 are tiny lipid bubbles in nanoparticle size that express the ACE2 protein, like handles for the virus to grab. These vesicles act as decoys to lure the SARS-CoV-2 virus away from the ACE2 protein on cells, which is how the virus infects cells. The virus spike protein grabs evACE2 instead of cellular ACE2, preventing it from entering the cell. Once captured, the virus will either float harmlessly around or be cleared by a macrophage immune cell. It can no longer cause infection.
“The key takeaway from this study is the identification of naturally occurring extracellular vesicles in the body that express the ACE2 receptor on their surface and serve as part of the normal adaptive defense against COVID-19-causing viruses,” said co-senior author Raghu Kalluri, M.D., Ph.D., chair of Cancer Biology at MD Anderson. “Building upon this, we’ve discovered a way to harness this natural defense as a new potential therapy against this devastating virus.”
The COVID-19 pandemic has been extended and challenged by a constantly changing SARS-CoV-2 virus. One of the biggest challenges is the moving target of pathogenic coronavirus that constantly evolves into new virus strains (variants) with mutations. These new viral strains harbor various changes in the viral protein spike with high infection rates and increased breakthroughs due to vaccine inefficiencies and resistance to therapeutic monoclonal antibodies.
“Our studies demonstrate that extracellular vesicles act to neutralize SARS-CoV-2 infection and highlight the potential for extracellular vesicles to play a broader role in defense against other types of infection which could be exploited therapeutically,” said co-lead author Kathleen McAndrews, Ph.D., postdoctoral fellow in Cancer Biology at MD Anderson.
Northwestern and MD Anderson have a pending patent on evACE2. The goal is to collaborate with industry partners and develop evACE2 as a biological therapeutic product (nasal spray or injected therapeutics) for prevention and treatment of COVID-19. Liu and another co-senior author, Deyu Fang from pathology at Northwestern, have formed a startup company, Exomira, to take this patent and develop evACE2 as a therapeutic.
“It remains urgent to identify novel therapeutics,” Liu said. “We think evACE2 can meet the challenges and fight against broad strains of SARS-CoV-2 and future emerging coronaviruses to protect the immunocompromised (at least 2.7% of U.S. adults), the unvaccinated (94% in low-income countries and more than 30% in the U.S.) and even the vaccinated from breakthrough infections.”
A team of more than 30 authors collaborated on this work. They include four lead co-first authors Lamiaa El-Shennawy, Andrew Hoffmann and Nurmaa Dashzeveg, all from the Liu lab at Northwestern, and McAndrews from the Kalluri Lab of MD Anderson.
News
Drug-Coated Neural Implants Reduce Immune Rejection
Summary: A new study shows that coating neural prosthetic implants with the anti-inflammatory drug dexamethasone helps reduce the body’s immune response and scar tissue formation. This strategy enhances the long-term performance and stability of electrodes [...]
Scientists discover cancer-fighting bacteria that ‘soak up’ forever chemicals in the body
A family of healthy bacteria may help 'soak up' toxic forever chemicals in the body, warding off their cancerous effects. Forever chemicals, also known as PFAS (per- and polyfluoroalkyl substances), are toxic chemicals that [...]
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
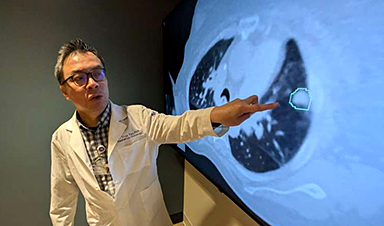
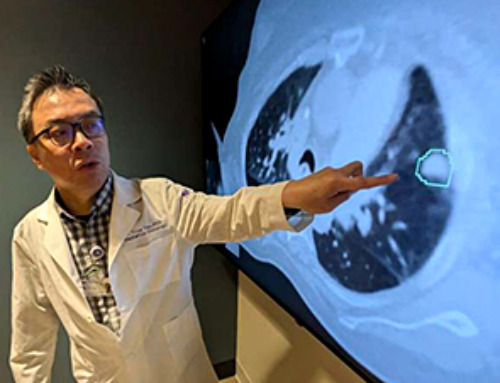
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
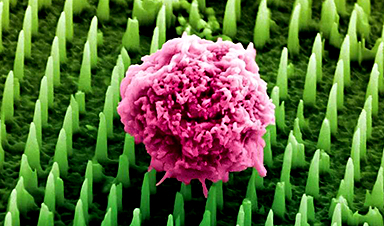
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]