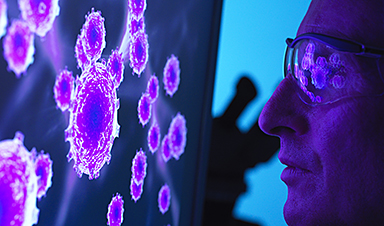
A team of researchers from the Institute for Infectious Diseases (IFIK) at the University of Bern and the Federal Institute of Virology and Immunology (IVI) have assessed virus growth and activation of the cellular defense mechanisms in the respiratory tract. They have shown that natural temperature differences that exist in the upper and lower respiratory tract have a profound influence on SARS-CoV-2 replication and subsequent innate immune activation in human cells. The findings can help to develop antiviral drugs and preventive measures.
“SARS-CoV-2 and SARS-CoV are highly similar genetically, generate a homologous repertoire of viral proteins, and use the same receptor to infect human cells. However, despite these similarities, there are also important differences between the two viruses,” says Ronald Dijkman from the Institute for Infectious Diseases (IFIK) at the University of Bern. For example, SARS-CoV infection is characterized by severe disease and inflammation in the lower respiratory tract and infected individuals are only contagious after the onset of symptoms, making it easier to identify and interrupt infection chains.
In contrast, SARS-CoV-2 preferentially replicates in the upper airways (nasal cavity, pharynx, trachea) and can be efficiently transmitted from one individual to another before the appearance of disease symptoms. Moreover, the outcome of SARS-CoV-2 infection varies widely from person to person, and can manifest as asymptomatic, mild, or severe disease. Older people as well as individuals with certain underlying medical conditions (heart conditions, diabetes, cancer) are at greater risk of developing severe illness, which is often associated with infection of lower respiratory tissues, high levels of inflammation, and lung failure.
Temperature is key
To better understand why infections with SARS-CoV and SARS-CoV-2 result in such different clinical outcomes, researchers from the University of Bern used specialized human airway cell cultures to investigate the impact of respiratory tract temperatures on SARS-CoV and SARS-CoV-2 replication. The cells originate from human samples and mimic the complexity of the cells found in the respiratory tract. They grow in special containers, are nourished from the bottom side and are exposed to air on the top side, just like the cells in the human trachea. The cultures also make mucus and have cilia that beat very quickly. “Because the organization of these cells greatly resembles the cells found in human tissues, they are a relevant system that can be used in a laboratory to study respiratory viruses,” Dijkman explains.
The researchers have now used this existing model for the first time to study the effects of respiratory temperatures on SARS-CoV and SARS-CoV-2 replication. They found that temperature plays an important role as SARS-CoV-2 preferred to replicate at temperatures typically found in the upper airways (33°C). Colder incubation temperatures allowed the virus to replicate faster and to a higher extent than when infections were carried out at 37°C to mimic the lower lung environment. Unlike SARS-CoV-2, replication of SARS-CoV was not impacted by different incubation temperatures. The experiments were conducted both in the high security laboratory of the IVI in Mittelhäusern and in the biosafety laboratory of the Institute for Infectious Diseases (IFIK) at the University of Bern in the building of sitem-insel, the Swiss Institute for Translational Medicine and Entrepreneurship.
Image Credit: Uni. of Bern
Post by Amanda Scott, NA CEO. Follow her on twitter @tantriclens
Thanks to Heinz V. Hoenen. Follow him on twitter: @HeinzVHoenen
News
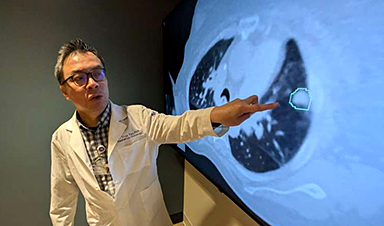
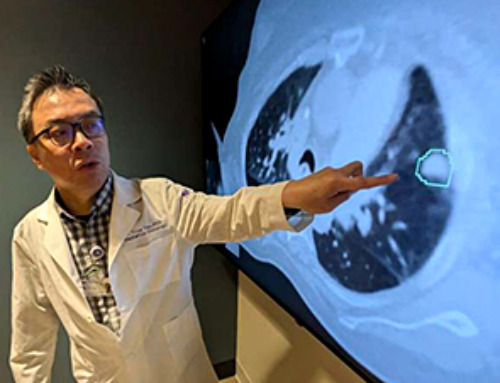
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
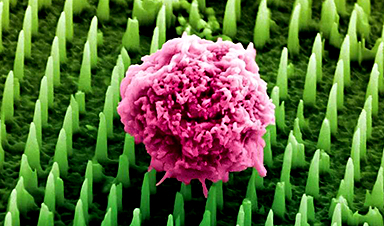
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
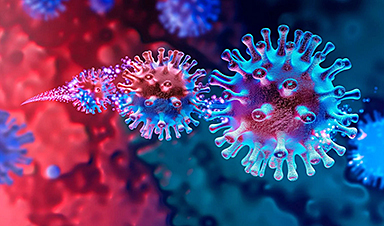
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
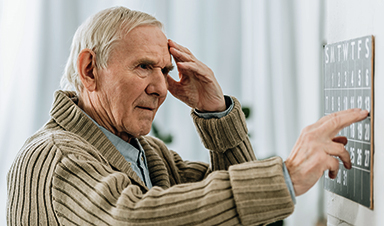
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]
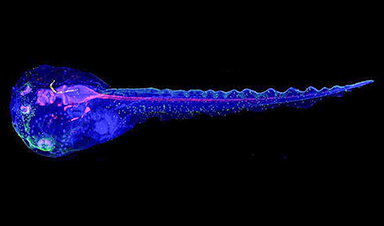
Cyborg tadpoles are helping us learn how brain development starts
How does our brain, which is capable of generating complex thoughts, actions and even self-reflection, grow out of essentially nothing? An experiment in tadpoles, in which an electronic implant was incorporated into a precursor [...]