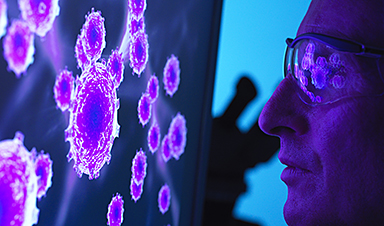
As COVID-19 approaches its fourth year, Omicron continues to mutate and become more immune-evasive, health officials say.
In December, the World Health Organization said variants descending from Omicron show more capacity to escape our immune system.
“Omicron, the latest variant of concern, is the most transmissible variant we have seen so far, including all the sub-variants that are in circulation,” Maria Van Kerkhove, WHO’s technical lead for COVID-19, said on Dec. 21.
Whether that’s enough to drive new waves of infections depends on conditions such as the size and timing of previous Omicron waves, the regional immune landscape and COVID-19 vaccination coverage, the United Nations public health agency said.
In Canada, differences in population-level immunity and global trends suggest COVID-19 cases could increase in the New Year, health officials said last week.
But what does mutation mean, what doesn’t it mean and why does immune evasiveness matter? Here are some answers based on what we know at this stage in the pandemic.
What’s a mutation?
A mutation is a change in the genetic code of the COVID-19 virus. Some mutations have no effect. Others lead to changes in proteins, which can be helpful to the virus by making it more transmissible — the ability to pass from one person to another. Or the mutation could be harmful to the virus if your immune system gains an advantage over the pathogen.
The WHO notes that there are currently about 540 Omicron mutations, but only five are “under monitoring” for changes such as mutations or rise in prevalence.
The variants of concern show one or several traits compared with the original or ancestral version of the virus:
- Spread more easily.
- Cause more severe illness.
- Evade or escape current vaccines or treatments.
In particular, physicians and scientists are watching for mutations to the virus’s spike protein. That’s what the virus uses to grab onto our cells and then enter them.
![]()
The BQ 1.1 subvariant of Omicron is immune evasive to the point where an antiviral treatment doesn’t work, Dr. Theresa Tam, Canada’s chief public health officer, said in mid December.
“We have to monitor susceptibility of the virus to these medications,” Tam said.
Genetic sequencing data also suggests the more immune-evasive variants are increasing, while BA.5 that dominated in the summer is decreasing, Tam said.
At a minimum, it means COVID cases will decline more slowly with a higher plateau of infections and hospitalizations as the respiratory virus season plays out, she said.
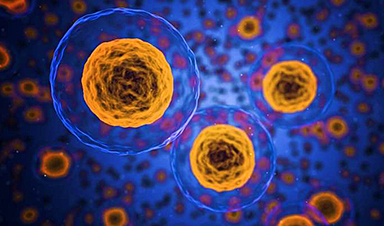
How does immunity work?
From the perspective of the virus, immunology professor Dawn Bowdish at McMaster University said if the virus allowed our immunity system to fend it off then it would be game over for the microbe. To survive, Omicron’s offspring variants like BQ1.1 skirt our immune defences.
The virus infects hosts to make copies of itself. In the process of using our cells as a virus factory, we get sick.
But not everyone who is exposed to the virus falls ill. As for why, think of the immune system like a medieval castle with different barriers, such as a wall surrounding the building, a moat and then armed guards.
First, there’s the outer wall to keep out invaders. For us, the main barrier to keep out respiratory pathogens is the nose. In the case of COVID-19, what scientists call “mucosal immunity” is found in the nasal passages and pharynx, commonly called the throat.
When the virus approaches, our natural immune response tries to summon for help.
“When they [Omicron subvariants] get into your nose, your mouth, when you first breathe them, they have ways of shutting off our natural antiviral immune responses,” said Bowdish, who holds the Canada Research Chair in aging and immunity.
Once the virus makes it through the first layer of defence, antibodies then act. Antibodies are proteins that your immune system makes to help fight infection. They also work to protect you from getting sick with the same virus in the future.
Antibodies need “to stick” to the virus to be effective, Bowdish said. Weeks after someone’s been vaccinated, the immune system produces lots of antibodies. Even if they don’t stick so well, the sheer number are likely to offer protection.
The tradeoff is that it takes us a lot of energy to make antibodies, which wane or decrease over weeks and months.
“In the context of Omicron, it’s well documented that the closer you are to your vaccine, the less likely you are to be infected with the virus because weeks after you receive your vaccine, your antibody levels are sky high,” Bowdish said.
COVID can evade immumity
But SARS-CoV-2, the virus that causes COVID-19, has other ways to overcome antibody defences.
“It’s also very good at hiding out from those antibodies,” Bowdish said.
Since Omicron subvariants evade the immune system’s capacity to fully control it, we’re more prone to re-infections now than with earlier variants, said Dr. Hélène Decaluwe, an immunologist and clinician-scientist.
“Most Canadians have been either infected or vaccinated,” said Decaluwe, who is also an associate professor at the University of Montreal. “Despite that, we cannot completely block the transmission.”
Decaluwe said antibody levels are an important way to block transmission, but their levels also decrease after a first infection.
“If you have your primary series of two vaccine doses and you have your booster with that third [dose], we can see in patients that have been infected [the combination] probably leads to better long-term memory of the infection,” she said.
That’s because the body’s immune system has been exposed to not only the viral spike protein but also others that are important to protect us from severe disease.
What happens when antibodies don’t protect us?
That’s what Decaluwe and her lab team research: T-cell response. T cells, a type of white blood cell that help protect the body from infection, are like the armed guards throwing spears at the COVID virus from the castle’s tower.
When antibodies fail to take care of the virus, T-cells kick in to prevent hospitalization and death from COVID-19 by targetting and destroying virus-infected cells. T cells do not prevent infection but set to work after a virus has penetrated.
Decaluwe and her colleagues with the Coronavirus Variants Rapid Response Network (CoVaRR-Net) use whole blood samples from nearly 600 individuals and advanced technology to study T-cell responses.
Decaluwe said about half of the subjects continue to provide blood samples to help researchers look at antibodies and other immune cells to detail the quality of their response.
Antibodies get created by another type of immune cells known as B cells.
When immune defences in the nose and antibodies aren’t efficient enough to block infection, then T-cells and B- cells enter the picture. One role of B-cells is to remember an invader to help make antibodies when reinfected. It’s as if B-cells are armed with a most-wanted poster to use their bow and arrows or catapults against Omicron.
Despite the advantages of the immune system and vaccinations, about 50 Canadians a week continue to die of COVID-19. Many of them are older than 65
Older individuals and those with immune compromising conditions are at increased risk of having severe COVID and are most in need of protective boosters, Decaluwe said.
Their vulnerability means medical researchers need to continue to keep watch for increased immune escape.
News
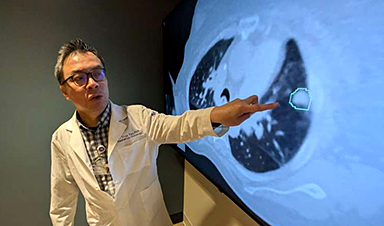
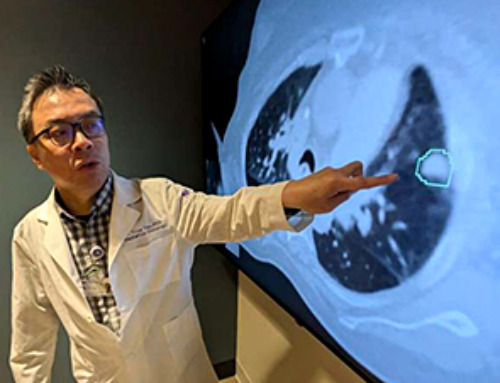
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
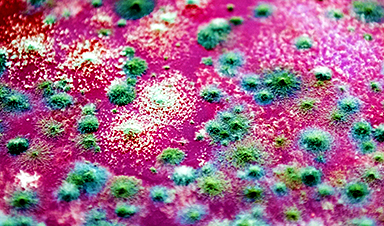
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
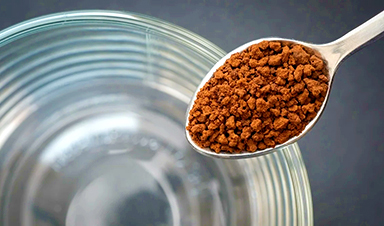
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
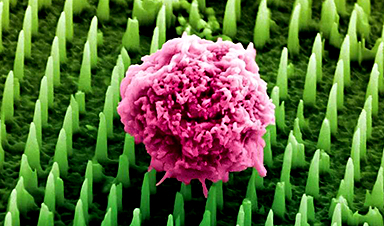
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]
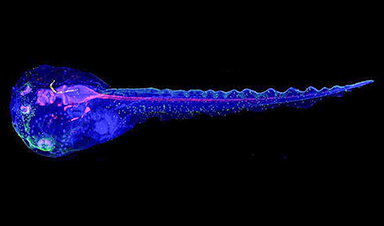
Cyborg tadpoles are helping us learn how brain development starts
How does our brain, which is capable of generating complex thoughts, actions and even self-reflection, grow out of essentially nothing? An experiment in tadpoles, in which an electronic implant was incorporated into a precursor [...]