Post-viral infection sequelae have included neurological syndromes. Among these is the association of parkinsonian manifestations with a prior history of viral infection, as far back as the Spanish flu pandemic of 1918, when encephalitis lethargica was recognized as a long-term complication of the flu. A new paper examines the possibility of similar syndromes following coronavirus disease 2019 (COVID-19).
Introduction
Viral infections sometimes affect non-target organs, including the brain, to cause neurological symptoms. With encephalitis lethargica, the mechanism was an imputed affinity of the virus for catecholamine-secreting neurons in the midbrain, specifically in the substantia nigra and locus ceruleus, two areas characteristically affected in Parkinson’s disease (PD). Inflammatory lesions or glial activation in the brain could also contribute to or account for the damage.
The ongoing COVID-19 pandemic was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has caused over 500 million cases globally. Though it causes mostly respiratory symptoms, other organs are also affected, directly or indirectly, as a result of the cytokine storm induced by the dysregulation of the immune-inflammatory response.
The authors of the current study, to be published online in the journal Movement Disorders, looked at the potential for an increased risk of parkinsonism following a bout of SARS-CoV-2 infection through accepted post-viral mechanisms. They used a mouse model that expressed the human angiotensin-converting enzyme 2 (hACE2) to study the neurological effects of the infection.
The animals were first infected with the virus at increasing titers. While the lower doses did not cause morbidity or mortality, the medium and higher doses were associated with symptoms and/or mortality in ~30% and 67% of cases.
The animals that died or were euthanized (when they lost 20% or more of their weight) appeared severely ill, but survivors remained euthermic and had normal blood oxygen levels. At 38 days after recovery, they were then inoculated to a mitochondrial poison, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), at subthreshold levels for toxicity. The aim was to induce some of the hallmark features of PD by the resulting low inflammation.
What did the study show?
The findings revealed that the recovered animals exposed to MPTP developed features of PD more readily compared to either the mice that were infected and recovered or were exposed to the chemical alone. No dopaminergic neuron loss was observed in any group other than the infection+MPTP group, which showed from a fifth to a quarter more damage than either the infection or the toxin alone.
When the striatal dopaminergic terminals alone were assessed, the differences were significant, with more than half being lost after MPTP use alone or associated with the infection, compared to the vehicle alone. In other words, despite the lower extent of dopaminergic neuron loss, the striatal terminal loss was comparable in both groups, indicating the greater sensitivity of the latter to oxidative stress induced by mitochondrial damage.
Microglial density was assessed in the resting and activated state in the dorsolateral striatum region in these groups. This showed marked differences between groups in the individual proportions of resting vs. activated microglia, though not the total number. That is, in the infection-MPTP group, resting microglia were reduced by over a third compared to any other. Active microglia were, meanwhile, increased by 300% in this group.
The density of activated microglia increased by ~110% and 180% in both MPTP groups, the former MPTP alone vs. vehicle alone and the latter infection-MPTP vs. infection alone.
What are the implications?
This study suggests the need to understand the risk of post-COVID-19 PD among the long-haulers and patients with long-term post-acute COVID-19 sequelae. In this study, it was clear that the infection alone did not cause either brain inflammation or death of dopaminergic neurons, ruling out direct viral toxicity as a cause of the PD. However, these neurons were sensitized by the infection to the injurious effects of mitochondrial stress, induced by a toxin at a level that is inadequate by itself to cause neuron loss.
This resembles the earlier reports of neurological sequelae to the flu pandemic. One study showed that humans who recovered from the Spanish flu were at a 73% higher risk of PD. In previous studies, the dose of MPTP was double that required to produce a dopaminergic loss in the present study. “This suggests that although different viruses can sensitize the brain to later insults, the dose of SARS-CoV-2 virus used here is a stronger sensitizing agent that the CA/09 H1N1 influenza virus.”
The mechanism appears to be via the cytokine storm induced by the presence of the virus, which leads to systemic inflammation. Thus, a transient increase in parkinsonian symptoms may be expected, but keeping in mind the increased sensitivity of these neurons to injury following SARS-CoV-2 infection vs. the flu.
During this upheaval, peripheral cytokines and chemokines may travel to the brain and cross the blood-brain barrier through the capillary beds while also influencing brain activity through the glymphatics of the brain. Inflammatory chemicals like these activate the innate immune system, viz, the astrocytes and microglia of the brain parenchyma. The result is further secretion of inflammatory proteins, creating a milieu in which the neurons are highly susceptible to further injury.
The highest microglial density compared to the neuronal density is in the striatal nucleus, the target of neurodegeneration in PD. This makes it especially vulnerable to oxidative damage from reactive oxygen radicals and mitochondrial injury. While the effects may be gradual rather than acute, the outcome is a persistent susceptibility to further injury that predisposes the cells to apoptosis or death following any kind of environmental or genetic insult.
Further research is necessary to understand the effects of the “second hit,” using other agents that act on other parts of the mitochondria. Again, the impact of COVID-19 vaccination or treatment on future neurological sequelae remains to be identified because the flu shots and the flu drug oseltamivir were both associated with eliminating the sensitizing effect of the second hit with MPTP.
Meanwhile, say the scientists, “for the more than 100 million people worldwide who survived COVID-19, without the benefit of access to vaccinations, the long-term consequences of infection, including increasing the risk for developing Parkinson’s disease, need to be understood. It is also critical for our healthcare providers and governmental agencies to prepare for this potential.”
News
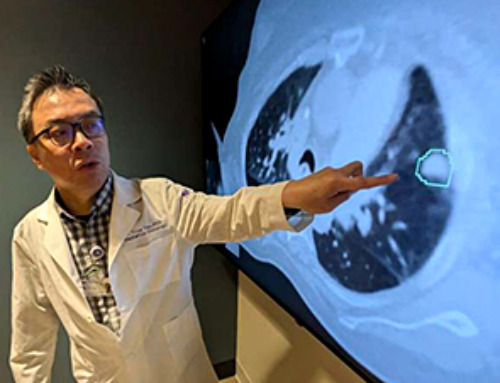
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
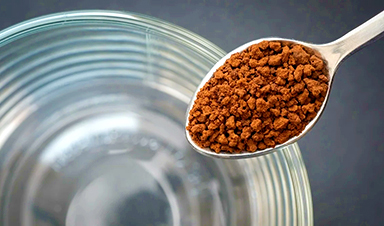
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
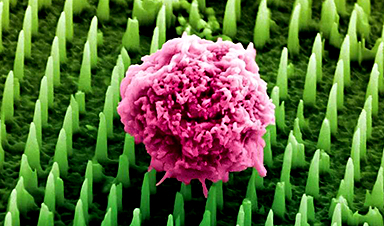
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
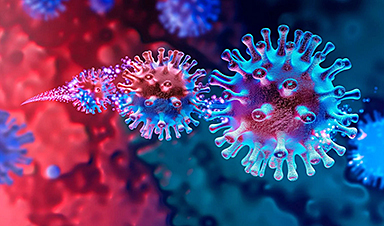
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
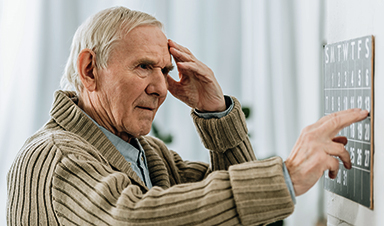
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]
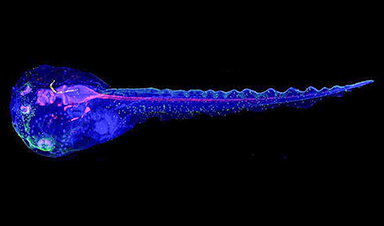
Cyborg tadpoles are helping us learn how brain development starts
How does our brain, which is capable of generating complex thoughts, actions and even self-reflection, grow out of essentially nothing? An experiment in tadpoles, in which an electronic implant was incorporated into a precursor [...]