Researchers in the United States have conducted a study showing that the coronavirus disease 2019 (COVID-19) vaccines developed by Pfizer-BioNTech and Moderna generate a coordinated adaptive immune response that is capable of eliciting recall responses to future infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The team from the University of California found that immunization with either Pfizer-BioNTech’s BNT162b2 or Moderna’s mRNA-1273 vaccine-induced enrichment of spike-specific B cells.
The viral spike protein mediates the initial stage of the SARS-CoV-2 infection process and is the primary target of antibodies following natural infection or vaccination.
Ilhem Messaoudi and colleagues say that vaccination also activated CD4 T cells and induced robust antigen-specific polyfunctional CD4 T cell responses.
Furthermore, clonally expanded CD8 T cells were observed in all vaccine recipients.
A pre-print version of the research paper is available on the bioRxiv* server, while the article undergoes peer review.
Vaccination and infection provide two different pathways to immunity
Since the COVID-19 outbreak first began in December 2019 in Wuhan, China, intense global efforts to rapidly develop effective vaccines against the causative agent SARS-CoV-2 have led to the emergency use authorization of several vaccines.
These include the messenger RNA- (mRNA) based vaccines developed by Pfizer (BNT162b2) and Moderna (mRNA-1273). Findings from clinical trials indicated that a 95% maximal protection is achieved within 1 to 2 months following the second dose of either vaccine, including protection against several circulating SARS-CoV-2 variants of concern.
However, the mechanisms by which these vaccines elicit long-lasting cellular immune responses to the virus remain poorly understood.
Natural infection and vaccination provide two different pathways to immunity, which studies have previously shown to be characterized by distinct T and B cell responses.
“Additional studies that integrate functional, transcriptional, and repertoire analysis of the memory immune cell response to COVID-19 mRNA vaccination are needed,” writes Messaoudi and colleagues.
What did the researchers do?
The team used single-cell RNA sequencing and functional assays to assess humoral (antibody) and cellular responses to two doses of either the Pfizer-BioNTech or Moderna mRNA vaccine (14 days following a second dose) in four individuals. The results were compared with the immune responses observed in three convalescent individuals who had experienced asymptomatic or mild infection.
What did the study find?
Both infection and vaccination induced anti-SARS-CoV-2 binding and neutralizing antibodies.
These antibodies were detected as early as two weeks following a first vaccine dose, with levels increasing several-fold after a second dose.
While neutralizing antibody titers following the first vaccine dose were comparable to those among convalescent individuals, significantly higher levels were observed in the vaccinees following the booster dose.
However, several important B cell adaptations were shared between vaccinees and convalescent individuals.
Analysis by flow cytometry revealed a reduction in the level of naïve B cells, but an expansion of memory B cells in both groups.
Additionally, single-cell RNA sequencing showed a reduction in IgA+ memory B cells following vaccination, a finding that has recently been described for convalescent individuals.
News
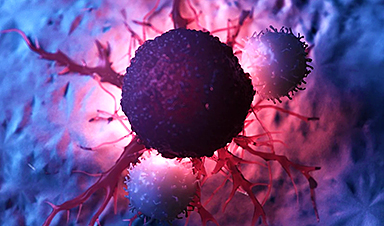
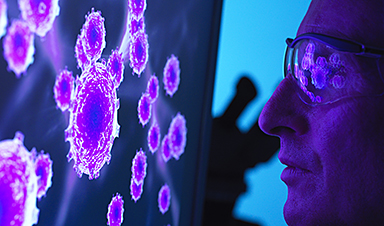
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
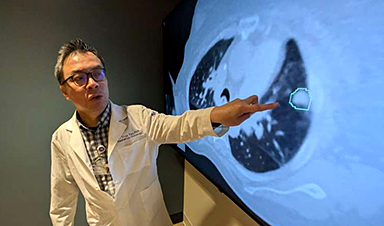
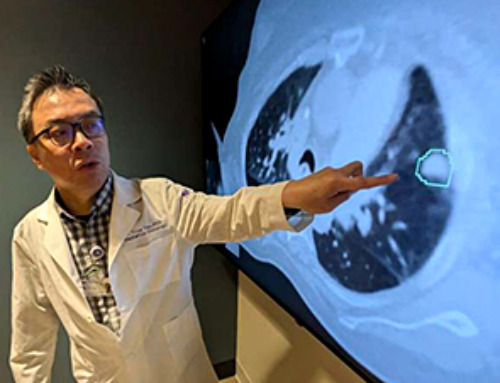
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
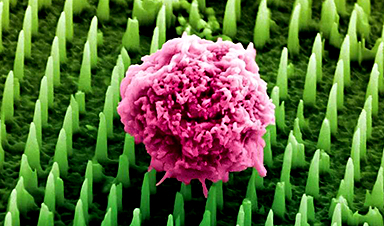
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]