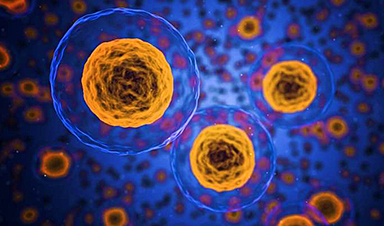
Tracking the pathway to immunity, one cell at a time.
Vaccines work their magic by effectively producing immune cells that survive for a long time, often for over decades. These immune cells build a barrier of protection that can prevent or minimize re-infection as well as a memory that enables us to identify a past invader like a virus and to eliminate it before it causes disease. The antibody in our blood that serves as the barrier is manufactured by “long-lived plasma cells”. While the significance of these cells has long been understood, how and when they are produced after vaccination has remained a mystery.
Until now.
A research team led by Dr. Marcus Robinson and Professor David Tarlinton from Monash University’s Immunological Memory Laboratory has shown in real time how immune memory cells are stored in the bone marrow at a rate of around one cell per hour for several weeks following vaccination. The findings were recently published in the journal Science Immunology. The researchers utilized a genetic system in mice to map the gradual accumulation of these cells.
After receiving a vaccination we remain largely immune to that disease because our bodies provide an ongoing supply of antibodies against the immunized disease – essentially making sure we remain topped up with these antibodies.
While we have known the sites in the body where these long-lived plasma cells have been generated including lymph nodes, tonsils, and gut – just what makes some vaccines lead to these cells sticking around for decades versus those that disappear after a few months has been unknown. Given the global interest in long-term immunity provided by COVID vaccines, there is an increased urgency in understanding this process.
Using a mouse model that expressed a fluorescent protein (called the TdTomato protein) only in cells specifically producing antibodies against a specific vaccine.
Because these cells fluoresced it was possible to track individual cells as they were produced and where they were stored.
The research used a series of tools to identify only those plasma cells that were generated by the vaccine. All plasma cells in the mouse model expressed a fluorescent protein (called TdTomato protein), and among those, they identified those recognizing the vaccine and finally, by using the timestamp, they knew when those cells had been made and thus how old they were.
According to Professor Tarlinton, studying these individual cells as they are born, mature, and get stored to protect us against repeat invasion by a particular virus or bacteria “can inform our understanding of how the recruitment of long-lived plasma cells occurs.”
The intricacy of the study has allowed the researchers to determine other aspects of the building up of specific immunity:
- How these plasma cells enter the bone marrow
- Whether these plasma cells must displace other cells when they get stored in areas such as bone marrow
- Or if these cells “find” a niche made vacant by previous plasma cells either dying or moving elsewhere
Mapping of these cells revealed that one particular vaccination in a mouse led to the generation of around 40,000 persisting plasma cells in the bone marrow. These cells, after the initial flourish, then decline at a rate of around 0.1% a day with a half-life of about 700 days, providing both an estimate of the duration of protection and identifying for further study the long-lived cells themselves.
According to Professor Tarlinton, understanding how these long-lived plasma cells are generated, live, and die “will inform our ability to modulate their recruitment, through different vaccine combinations or delivery strategies – ultimately allowing us to be able to increase the longevity of immunity,” he said.
“In fact, there is exciting work recently reported in Nature that describes how altering the mechanics of vaccination can dramatically influence the character of the immune response, and we would predict the production of these special cells that have been the focus of our work.”
News
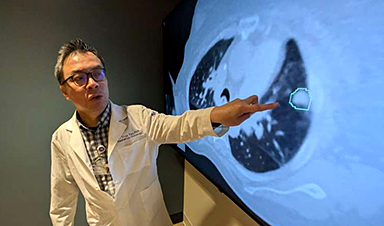
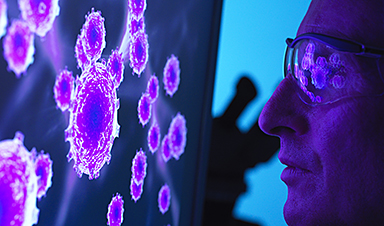
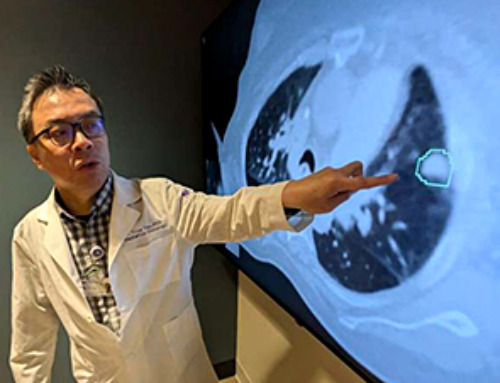
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
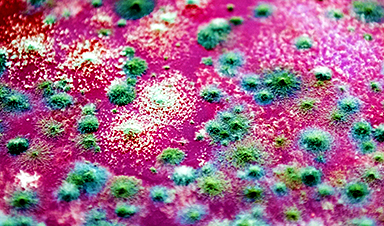
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
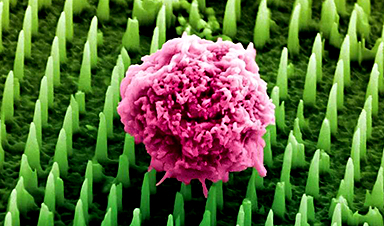
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
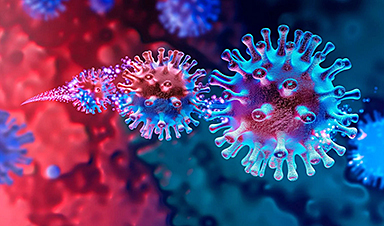
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
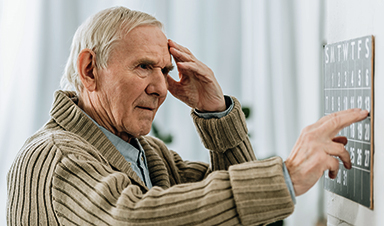
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]
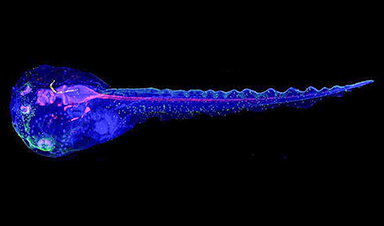
Cyborg tadpoles are helping us learn how brain development starts
How does our brain, which is capable of generating complex thoughts, actions and even self-reflection, grow out of essentially nothing? An experiment in tadpoles, in which an electronic implant was incorporated into a precursor [...]