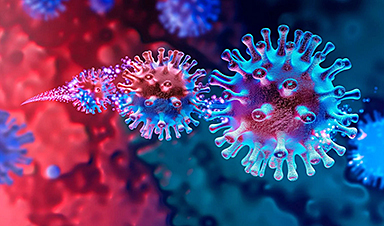
In a recent study published in npj Vaccines, a group of researchers demonstrated that a single-dose intranasal application of a modified Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) strain ∆3678 effectively induces robust immune responses, protecting mice against various forms of the virus, suggesting its potential as an efficient mucosal vaccine.
Background
Over three years, SARS-CoV-2, the instigator of the coronavirus disease 2019 (COVID-19) pandemic, has claimed over 6.9 million lives globally. Despite the expedited creation of four Food and Drug Administration (FDA)-authorized vaccines, their efficacy is threatened by emerging, more transmissible variants known for immune evasion.
The current vaccines, delivered via injection, can potentially provoke insufficient respiratory tract immune reactions, especially against these variants. Intranasal immunization can stimulate robust local and systemic immunity, offering enhanced protection.
Further research is essential due to the ongoing global health threat posed by SARS-CoV-2 variants and the limited respiratory tract immune responses induced by current parenterally administered vaccines, underscoring the need for an optimized intranasal vaccine that effectively bolsters both mucosal and systemic immunity.
About the study
The researchers cultivated Vero-E6 cells from African green monkeys and Vero-E6-TMPRSS2 cells, maintaining them at 37°C with 5% CO2.
They used infectious clones of SARS-CoV-2, ∆3678, and the BA.5 variant. For animal studies, female K18-hACE2 C57BL/6J mice, aged 8-10 weeks, were infected intranasally (i.n.) with either the WT WA1 or ∆3678 viruses or mock-infected.
On day 28 post-initial infection, they were challenged with the WT WA1 or BA.5 virus. The researchers monitored the mice for weight changes and health status, euthanizing those losing over 20% of their body weight.
The University of Texas Medical Branch’s Institutional Animal Care and Use Committee sanctioned all experiments in an Animal Biosafety Level 3 (ABSL3) environment. Researchers processed lung lobes for plaque assays and utilized centrifugation for clarification.
They employed the Enzyme-Linked Immunosorbent Assay (ELISA) with SARS-CoV-2 Receptor-Binding Domain (RBD) protein for antibody detection. B cell Enzyme-Linked ImmunoSPOT (ELISPOT) assays adhered to known protocols. Lung leukocytes or splenocytes were also exposed to SARS-CoV-2 peptides for intracellular cytokine staining using specific antibodies.
Lung tissues were subjected to RNA extraction and analyzed using the nCounter Pro System, with results visualized in R 4.1.2. Statistical evaluations of viral loads, cytokines, antibodies, and cell responses were performed using Prism software, employing non-paired Student’s t-tests for p-values.
Study results
In the present study, researchers employed K18-hACE2 mice to explore the potential of the ∆3678 virus as a vaccine against SARS-CoV-2, inspired by previous research. The mice received intranasal immunization with this attenuated strain, with groups administered wild-type SARS-CoV-2 USA-WA1/2020 or a placebo serving as controls.
Remarkably, all mice immunized with the ∆3678 virus thrived without signs of weight loss or ill health 28 days after vaccination, contrasting with some fatalities and weight loss in mice exposed to the wild-type virus.
When the researchers analyzed immune responses, they discovered both the ∆3678 and wild-type virus evoked a Th1-skewed response in the lungs. The ∆3678 group exhibited notable T cell activation, especially in the heightened presence and activity of CD4+ and CD8+ T cells producing Interferon Gamma (IFNγ).
Although both groups showed robust Immunoglobulin A (IgA)+ B cell responses, the ∆3678 groups were slightly diminished. Interestingly, both groups exhibited comparable SARS-CoV-2-specific IgA or IgG antibodies, with similar patterns observed in the spleen, indicating a systemic Th1-prone response.
The team then assessed the vaccine’s protective efficacy, exposing the immunized mice to a high dose of wild-type SARS-CoV-2, and observed that mice previously inoculated with either the ∆3678 or wild-type virus exhibited neither traces of the virus in their lungs or trachea nor weight loss following the challenge, contrasting with the control group.
Notably, even when challenged with the Omicron BA.5 variant, the ∆3678 group demonstrated no detectable viral presence, highlighting the vaccine’s broad protective potential.
Further analyses post-challenge revealed an enhanced immune response in ∆3678-immunized mice, particularly in the increased numbers of activated T cells in the lungs and spleen. Additionally, both vaccinated groups exhibited strong antibody responses.
Researchers analyzed lung tissue gene expression to decipher the immunity mechanisms, uncovering diminished inflammatory signaling in vaccinated groups and identifying genes linked to long-lasting lung-resident memory T-cell responses.
These findings collectively suggest the ∆3678 strain, though highly attenuated, effectively stimulates comprehensive immune responses in mice, even those previously exposed to SARS-CoV-2. The vaccine appears to confer solid protection against diverse SARS-CoV-2 strains, including the Omicron variant.
The promise shown by intranasal administration of this live-attenuated vaccine candidate in mice warrants further exploration, especially considering the potential for enhanced and sustained mucosal immunity.
However, its efficacy in humans requires further investigation. The profound insights gained from this study underline the ∆3678 virus as a compelling candidate for future SARS-CoV-2 vaccines, potentially impacting both human and veterinary medicine.
- Adam, A., Kalveram, B., Chen, J.YC. et al. (2023) A single-dose of intranasal vaccination with a live-attenuated SARS-CoV-2 vaccine candidate promotes protective mucosal and systemic immunity. npj Vaccines., doi: https://doi.org/10.1038/s41541-023-00753-4. https://www.nature.com/articles/s41541-023-00753-4
News
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
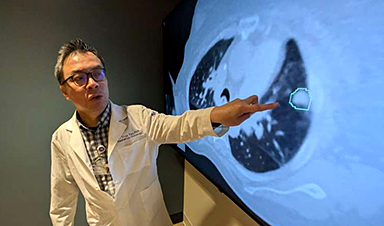
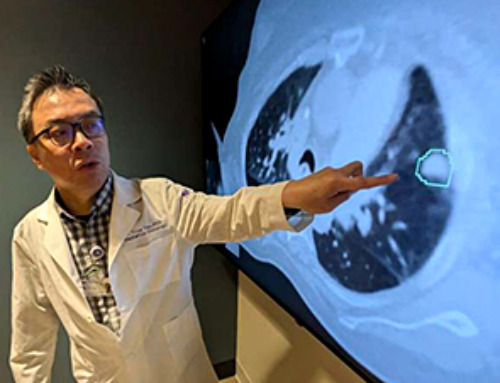
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
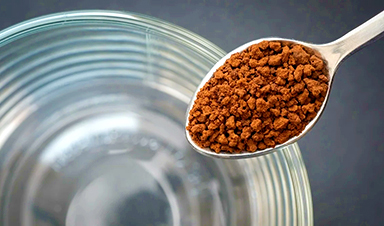
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
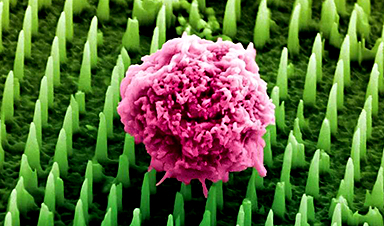
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]