In a recent study published in the journal PLOS ONE, researchers conducted a systematic review and meta-analyzed data on the impact of coronavirus disease 2019 (COVID-19) on male reproductive hormones and semen variables to determine whether severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections had an adverse impact on male fertility.
Background
The etiological agent of the COVID-19 pandemic, SARS-CoV-2, is a β-coronavirus that infects human cells by binding to the angiotensin-converting enzyme-2 (ACE-2) receptor. The ACE-2 receptor is found in the lungs, kidneys, heart, and testes, making all these organs possible entry points for the virus.
The COVID-19 pandemic was responsible for over 700 million cases and more than 7 million deaths. However, although the virus is known to primarily infect the respiratory system, research indicates that it can also adversely impact other organ systems. Studies have also found that SARS-CoV-2 infections are more severe in males than in females. Furthermore, studies have found that many males who had been infected with the earlier SARS-CoV-1 had developed orchitis or inflammation of the testes.
However, the data on the impact of SARS-CoV-2 on male reproductive health has been limited. Although some studies have reported associations between COVID-19 and decreased testosterone levels and lower semen quality, some of the findings have been considered methodologically weak.
About the study
The present study aimed to comprehensively review recent studies examining the impact of COVID-19 on male fertility and conducted a meta-analysis by comparing semen quality variables and reproductive hormone levels between infected and uninfected men to understand the influence of SARS-CoV-2 on male fertility.
The researchers used the PECO, or Population, Exposure, Comparator, and Outcomes, model to select studies that examined male patients of reproductive age who had been exposed to SARS-CoV-2. The review included both prospective and retrospective studies as long as they included COVID-19-negative controls or contained pre- and post-COVID-19 pandemic health data for the same individual. Studies that were in vitro, focused on female patients, or lacking control groups were excluded.
For the studies included in the review, the outcomes consisted of measurements of conventional semen parameters such as sperm count, ejaculate volume, sperm concentration, morphology, motility, and viability of the sperm, as well as leukocyte levels in the seminal fluid. The outcomes also included the levels of the male reproductive hormones, including testosterone, estrogen, prolactin, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). The Measurements also included ratios of testosterone to LH and FSH to LH.
For the meta-analysis, the data extracted from the studies consisted of sample sizes, country of study, study design, the methods used to diagnose COVID-19, and key outcomes. The researchers used this data to calculate standardized mean differences, with extensive sensitivity analyses to avoid bias and assess sources of diversity. The parameters were also compared for changes before and after treatment for COVID-19.
Results
The review identified 40 eligible studies published from 12 different countries between 2020 and 2023 that examined the impact of SARS-CoV-2 on male reproductive health. The key findings from the meta-analysis covered the impact of COVID-19 on several aspects of male reproductive health.
The study found that COVID-19 was significantly associated with decreased ejaculate volume, with sensitivity analyses confirming consistent reductions in ejaculate volume after SARS-CoV-2 infections. However, the sensitivity analyses showed that the difference in ejaculate volume before and after COVID-19 treatment was not statistically significant, indicating that the impact of treatment may be limited. The sperm counts also decreased after SARS-CoV-2 infections, although the sensitivity analyses indicated that these reductions were marginal.
Individuals infected with SARS-CoV-2 also showed significantly lower sperm concentrations, and no changes were seen in sperm concentrations after treatment for COVID-19. This finding remained consistent even after accounting for potential study biases and diversity, reinforcing the robustness of the result. COVID-19 was also found to lower sperm viability and motility, with the difference in sperm viability remaining consistent even after the sensitivity analysis.
Comparisons between infected and uninfected individuals revealed no significant differences in sperm morphology. However, comparisons of sperm morphology in the same individual before and after SARS-CoV-2 infections revealed lower levels of morphologically normal sperm. The analysis showed that while the overall morphology differences between infected and uninfected individuals were not significant, the within-individual changes suggest that SARS-CoV-2 may have a subtle but noteworthy effect on sperm morphology.
The reproductive hormone levels were also significantly altered in COVID-19 patients, with elevated prolactin and marginally higher estrogen levels in infected men. Interestingly, the study found substantial variability in testosterone levels before and after treatment, suggesting that COVID-19’s impact on this hormone may be more complex than initially understood. However, the leukocyte levels in the seminal fluid were similar between infected and uninfected men.
Conclusions
To summarize, the study reviewed and conducted a meta-analysis of studies examining the impact of COVID-19 on male reproductive health and found that SARS-CoV-2 had a significant negative impact on male fertility, particularly on parameters such as ejaculate volume, viability, and motility of the sperm, and sperm concentration and count. Although the treatment of COVID-19 partially alleviated some of the affected parameters, the findings suggest that these improvements may not be sufficient to restore pre-infection levels, particularly for parameters like sperm concentration and motility. The study also highlighted the need for further research to fully understand the long-term effects of COVID-19 on male fertility and to explore potential therapeutic interventions.
- V. J., Ashonibare, P. J., Ashonibare, T. M., Akhigbe, & E, A. R. (2024). SARS-CoV-2 impairs male fertility by targeting semen quality and testosterone level: A systematic review and meta-analysis. PLOS ONE, 19(9), e0307396-. DOI:10.1371/journal.pone.0307396, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0307396
News
Scientists Develop IV Therapy That Repairs the Brain After Stroke
New nanomaterial passes the blood-brain barrier to reduce damaging inflammation after the most common form of stroke. When someone experiences a stroke, doctors must quickly restore blood flow to the brain to prevent death. [...]
Analyzing Darwin’s specimens without opening 200-year-old jars
Scientists have successfully analyzed Charles Darwin's original specimens from his HMS Beagle voyage (1831 to 1836) to the Galapagos Islands. Remarkably, the specimens have been analyzed without opening their 200-year-old preservation jars. Examining 46 [...]
Scientists discover natural ‘brake’ that could stop harmful inflammation
Researchers at University College London (UCL) have uncovered a key mechanism that helps the body switch off inflammation—a breakthrough that could lead to new treatments for chronic diseases affecting millions worldwide. Inflammation is the [...]
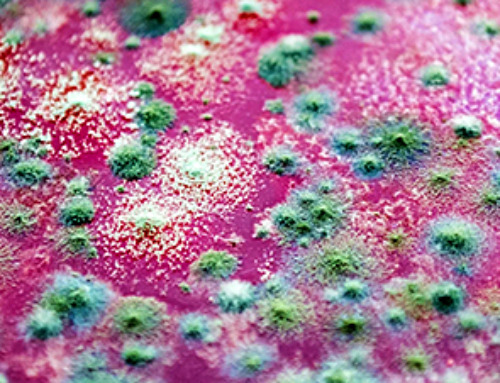
A Forgotten Molecule Could Revive Failing Antifungal Drugs and Save Millions of Lives
Scientists have uncovered a way to make existing antifungal drugs work again against deadly, drug-resistant fungi. Fungal infections claim millions of lives worldwide each year, and current medical treatments are failing to keep pace. [...]
Scientists Trap Thyme’s Healing Power in Tiny Capsules
A new micro-encapsulation breakthrough could turn thyme’s powerful health benefits into safer, smarter nanodoses. Thyme extract is often praised for its wide range of health benefits, giving it a reputation as a natural medicinal [...]
Scientists Develop Spray-On Powder That Instantly Seals Life-Threatening Wounds
KAIST scientists have created a fast-acting, stable powder hemostat that stops bleeding in one second and could significantly improve survival in combat and emergency medicine. Severe blood loss remains the primary cause of death from [...]
Oceans Are Struggling To Absorb Carbon As Microplastics Flood Their Waters
New research points to an unexpected way plastic pollution may be influencing Earth’s climate system. A recent study suggests that microscopic plastic pollution is reducing the ocean’s capacity to take in carbon dioxide, a [...]
Molecular Manufacturing: The Future of Nanomedicine – New book from Frank Boehm
This book explores the revolutionary potential of atomically precise manufacturing technologies to transform global healthcare, as well as practically every other sector across society. This forward-thinking volume examines how envisaged Factory@Home systems might enable the cost-effective [...]
New Book! NanoMedical Brain/Cloud Interface – Explorations and Implications
New book from Frank Boehm, NanoappsMedical Inc Founder: This book explores the future hypothetical possibility that the cerebral cortex of the human brain might be seamlessly, safely, and securely connected with the Cloud via [...]
Global Health Care Equivalency in the Age of Nanotechnology, Nanomedicine and Artificial Intelligence
A new book by Frank Boehm, NanoappsMedical Inc. Founder. This groundbreaking volume explores the vision of a Global Health Care Equivalency (GHCE) system powered by artificial intelligence and quantum computing technologies, operating on secure [...]
Miller School Researchers Pioneer Nanovanilloid-Based Brain Cooling for Traumatic Injury
A multidisciplinary team at the University of Miami Miller School of Medicine has developed a breakthrough nanodrug platform that may prove beneficial for rapid, targeted therapeutic hypothermia after traumatic brain injury (TBI). Their work, published in ACS [...]
COVID-19 still claims more than 100,000 US lives each year
Centers for Disease Control and Prevention researchers report national estimates of 43.6 million COVID-19-associated illnesses and 101,300 deaths in the US during October 2022 to September 2023, plus 33.0 million illnesses and 100,800 deaths [...]
Nanomedicine in 2026: Experts Predict the Year Ahead
Progress in nanomedicine is almost as fast as the science is small. Over the last year, we've seen an abundance of headlines covering medical R&D at the nanoscale: polymer-coated nanoparticles targeting ovarian cancer, Albumin recruiting nanoparticles for [...]
Lipid nanoparticles could unlock access for millions of autoimmune patients
Capstan Therapeutics scientists demonstrate that lipid nanoparticles can engineer CAR T cells within the body without laboratory cell manufacturing and ex vivo expansion. The method using targeted lipid nanoparticles (tLNPs) is designed to deliver [...]
The Brain’s Strange Way of Computing Could Explain Consciousness
Consciousness may emerge not from code, but from the way living brains physically compute. Discussions about consciousness often stall between two deeply rooted viewpoints. One is computational functionalism, which holds that cognition can be [...]
First breathing ‘lung-on-chip’ developed using genetically identical cells
Researchers at the Francis Crick Institute and AlveoliX have developed the first human lung-on-chip model using stem cells taken from only one person. These chips simulate breathing motions and lung disease in an individual, [...]