A recent study conducted by scientists at the University of Southern California sheds light on the reasons why children are not receiving an affordable and effective diarrhea treatment.
Medical professionals in developing nations are aware that oral rehydration salts (ORS), a cost-effective treatment, can save lives by treating diarrheal diseases, which are among the top causes of mortality for children globally. Despite this, few prescribe it.
A new study published in Science suggests that closing the knowledge gap between what treatments healthcare providers think patients want and what treatments patients really want could help save half a million lives a year and reduce unnecessary use of antibiotics.
“Even when children seek care from a health care provider for their diarrhea, as most do, they often do not receive ORS, which costs only a few cents and has been recommended by the World Health Organization for decades,” said Neeraj Sood, senior author of the study, a senior fellow at the USC Schaeffer Center for Health Policy & Economics and a professor at the USC Price School of Public Policy.
“This issue has puzzled experts for decades, and we wanted to get to the bottom of it,” said Sood, who also holds joint appointments at the Keck School of Medicine of USC and the USC Marshall School of Business.
A closer look at childhood illness in India
There are several popular explanations for the underprescription of ORS in India, which accounts for the most cases of child diarrhea of any country in the world:
- Physicians assume their patients do not want oral rehydration salts, which come in a small packet and dissolve in water, because they taste bad or they aren’t “real” medicine like antibiotics.
- The salts are out of stock because they aren’t as profitable as other treatments.
- Physicians make more money prescribing antibiotics, even though they are ineffective against viral diarrhea.
To test these three hypotheses, Sood and his colleagues enrolled over 2,000 healthcare providers across 253 medium-size towns in the Indian states of Karnataka and Bihar. The researchers selected states with vastly different socioeconomic demographics and varied access to health care to ensure the results were representative of a broad population. Bihar is one of the poorest states in India with below-average ORS use, while Karnataka has above-average per capita income and above-average ORS use.
Neeraj Sood, PhD, senior fellow at the USC Schaeffer Center for Health Policy & Economics and professor at the USC Price School of Public Policy, presents the study’s key findings. Credit: University of Southern California
The researchers then hired staff who were trained to act as patients or caretakers. These “standardized patients” were given scripts to use in unannounced visits to doctors’ offices where they would present a case of viral diarrhea — for which antibiotics are not appropriate — in their 2-year-old child. (For ethical considerations, children did not attend these visits.) The standardized patients made approximately 2,000 visits in total.
Providers were randomly assigned to patient visits where patients expressed a preference for ORS, a preference for antibiotics, or no treatment preference. During the visits, patients indicated their preference by showing the healthcare provider a photo of an ORS packet or antibiotics. The set of patients with no treatment preference simply asked the physician for a recommendation.
To control for profit-motivated prescribing, some of the standardized patients assigned as having no treatment preference informed the provider that they would purchase medicine elsewhere. Additionally, to estimate the effect of stockouts, the researchers randomly assigned all providers in half of the 253 towns to receive a six-week supply of ORS.
Provider misperceptions matter most when it comes to ORS underprescribing
Researchers found that provider perceptions of patient preferences are the biggest barrier to ORS prescribing — not because caretakers do not want ORS, but rather because providers assume most patients do not want the treatment. Healthcare providers’ perception that patients do not want ORS accounted for roughly 42% of underprescribing, while stockouts and financial incentives explained only 6% and 5%, respectively.
Patients expressing a preference for ORS increased prescribing of the treatment by 27 percentage points — a more effective intervention than eliminating stockouts (which increased ORS prescribing by 7 percentage points) or removing financial incentives (which only increased ORS prescribing at pharmacies).
“Despite decades of widespread knowledge that ORS is a lifesaving intervention that can save lives of children suffering from diarrhea, the rates of ORS use remain stubbornly low in many countries such as India,” said Manoj Mohanan, co-author of the study and professor of public policy, economics, and global health at the Sanford School of Public Policy at Duke University. “Changing provider behavior about ORS prescription remains a huge challenge.”
Study authors said these results can be used to design interventions that encourage patients and caretakers to express an ORS preference when seeking care, as well as efforts to raise awareness among providers about patients’ preferences.
“We need to find ways to change providers’ perceptions of patient preferences to increase ORS use and combat antibiotic resistance, which is a huge problem globally,” said Zachary Wagner, the study’s corresponding author, an economist at RAND Corporation and professor of policy analysis at Pardee RAND Graduate School. “How to reduce overprescribing of antibiotics and address antimicrobial resistance is a major global health question, and our study shows that changing provider perceptions of patient preferences is one way to work toward a solution.”
Reference: “What drives poor quality of care for child diarrhea? Experimental evidence from India” by Zachary Wagner, Manoj Mohanan, Rushil Zutshi, Arnab Mukherji and Neeraj Sood, 9 February 2024, Science.
DOI: 10.1126/science.adj9986
This research was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (Grant 5R01DK126049).
News
Johns Hopkins Researchers Uncover a New Way To Kill Cancer Cells
A new study reveals that blocking ribosomal RNA production rewires cancer cell behavior and could help treat genetically unstable tumors. Researchers at the Johns Hopkins Kimmel Cancer Center and the Department of Radiation Oncology and Molecular [...]
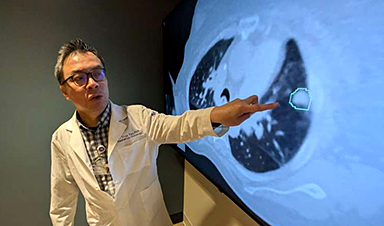
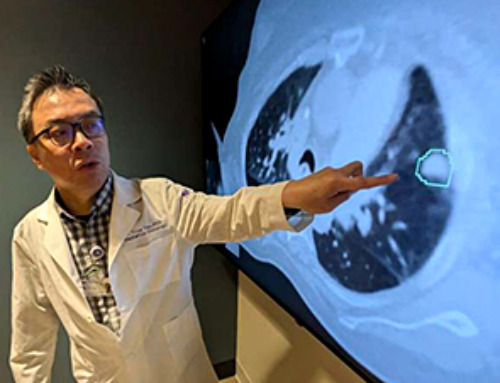
AI matches doctors in mapping lung tumors for radiation therapy
In radiation therapy, precision can save lives. Oncologists must carefully map the size and location of a tumor before delivering high-dose radiation to destroy cancer cells while sparing healthy tissue. But this process, called [...]
Scientists Finally “See” Key Protein That Controls Inflammation
Researchers used advanced microscopy to uncover important protein structures. For the first time, two important protein structures in the human body are being visualized, thanks in part to cutting-edge technology at the University of [...]
AI tool detects 9 types of dementia from a single brain scan
Mayo Clinic researchers have developed a new artificial intelligence (AI) tool that helps clinicians identify brain activity patterns linked to nine types of dementia, including Alzheimer's disease, using a single, widely available scan—a transformative [...]
Is plastic packaging putting more than just food on your plate?
New research reveals that common food packaging and utensils can shed microscopic plastics into our food, prompting urgent calls for stricter testing and updated regulations to protect public health. Beyond microplastics: The analysis intentionally [...]
Aging Spreads Through the Bloodstream
Summary: New research reveals that aging isn’t just a local cellular process—it can spread throughout the body via the bloodstream. A redox-sensitive protein called ReHMGB1, secreted by senescent cells, was found to trigger aging features [...]
AI and nanomedicine find rare biomarkers for prostrate cancer and atherosclerosis
Imagine a stadium packed with 75,000 fans, all wearing green and white jerseys—except one person in a solid green shirt. Finding that person would be tough. That's how hard it is for scientists to [...]
Are Pesticides Breeding the Next Pandemic? Experts Warn of Fungal Superbugs
Fungicides used in agriculture have been linked to an increase in resistance to antifungal drugs in both humans and animals. Fungal infections are on the rise, and two UC Davis infectious disease experts, Dr. George Thompson [...]
Scientists Crack the 500-Million-Year-Old Code That Controls Your Immune System
A collaborative team from Penn Medicine and Penn Engineering has uncovered the mathematical principles behind a 500-million-year-old protein network that determines whether foreign materials are recognized as friend or foe. How does your body [...]
Team discovers how tiny parts of cells stay organized, new insights for blocking cancer growth
A team of international researchers led by scientists at City of Hope provides the most thorough account yet of an elusive target for cancer treatment. Published in Science Advances, the study suggests a complex signaling [...]
Nanomaterials in Ophthalmology: A Review
Eye diseases are becoming more common. In 2020, over 250 million people had mild vision problems, and 295 million experienced moderate to severe ocular conditions. In response, researchers are turning to nanotechnology and nanomaterials—tools that are transforming [...]
Natural Plant Extract Removes up to 90% of Microplastics From Water
Researchers found that natural polymers derived from okra and fenugreek are highly effective at removing microplastics from water. The same sticky substances that make okra slimy and give fenugreek its gel-like texture could help [...]
Instant coffee may damage your eyes, genetic study finds
A new genetic study shows that just one extra cup of instant coffee a day could significantly increase your risk of developing dry AMD, shedding fresh light on how our daily beverage choices may [...]
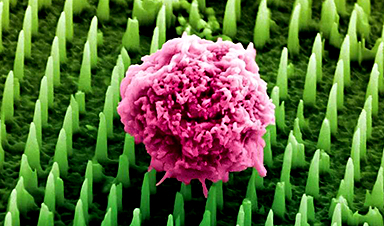
Nanoneedle patch offers painless alternative to traditional cancer biopsies
A patch containing tens of millions of microscopic nanoneedles could soon replace traditional biopsies, scientists have found. The patch offers a painless and less invasive alternative for millions of patients worldwide who undergo biopsies [...]
Small antibodies provide broad protection against SARS coronaviruses
Scientists have discovered a unique class of small antibodies that are strongly protective against a wide range of SARS coronaviruses, including SARS-CoV-1 and numerous early and recent SARS-CoV-2 variants. The unique antibodies target an [...]
Controlling This One Molecule Could Halt Alzheimer’s in Its Tracks
New research identifies the immune molecule STING as a driver of brain damage in Alzheimer’s. A new approach to Alzheimer’s disease has led to an exciting discovery that could help stop the devastating cognitive decline [...]