Twenty-five years ago, in 1998, researchers in Wisconsin isolated powerful stem cells from human embryos. It was a fundamental breakthrough for biology, since these cells are the starting point for human bodies and have the capacity to turn into any other type of cell—heart cells, neurons, you name it.
National Geographic would later summarize the incredible promise: “the dream is to launch a medical revolution in which ailing organs and tissues might be repaired” with living replacements. It was the dawn of a new era. A holy grail. Pick your favorite cliché—they all got airtime.
Yet today, more than two decades later, there are no treatments on the market based on these cells. Not one.
To find out what happened, this June I grabbed a seat in the front row at the annual International Society for Stem Cell Research meeting, in an auditorium alongside hundreds of biologists. Projected on a huge screen was a slightly intimidating black-and-white image of cells seen through a microscope, some round with groping hair-like extensions, others rectangular cross-sections filled with a mysterious substance that looked like sand. Theme music bubbled from the stage: “I Want a New Drug,” by Huey Lewis and the News.
Others concede that melding stem cells into medicine has proved surprisingly difficult. The basic challenge is that cells are not like aspirin or another drug that can be made by the pound. They’re living things, which can change, die, or even run out of control, causing dangers like cancer. By this account, capturing the embryonic stem cell was the easy part. It’s coaxing them to produce specialized cells—the kind with specific functions needed to treat disease—that’s been so hard.
“Ideas take a long time, but it’s still the right idea,” said Matthew Porteus, a professor from Stanford University whom I peppered with questions while he was standing at a podium at the meeting.
There are signs that stem-cell-based treatments are finally poised for a breakout. According to a 2023 survey, nearly 70 new tests on volunteers got underway in the last four years—triple the previous pace. One of these early human studies is being carried out by Vertex Pharmaceuticals, which in June said two diabetes patients who received injections of lab-made pancreatic cells no longer have to take insulin. Tests of manufactured cells to treat blindness and epilepsy also have early results that suggest transplanted cells are helping.
“A lot of things are on the verge,” says Haifan Lin, a Yale University professor who is the outgoing president of the ISSCR. “I don’t think it’s delayed, because stem cells are truly the most complicated of all cells.”
Tabula rasa
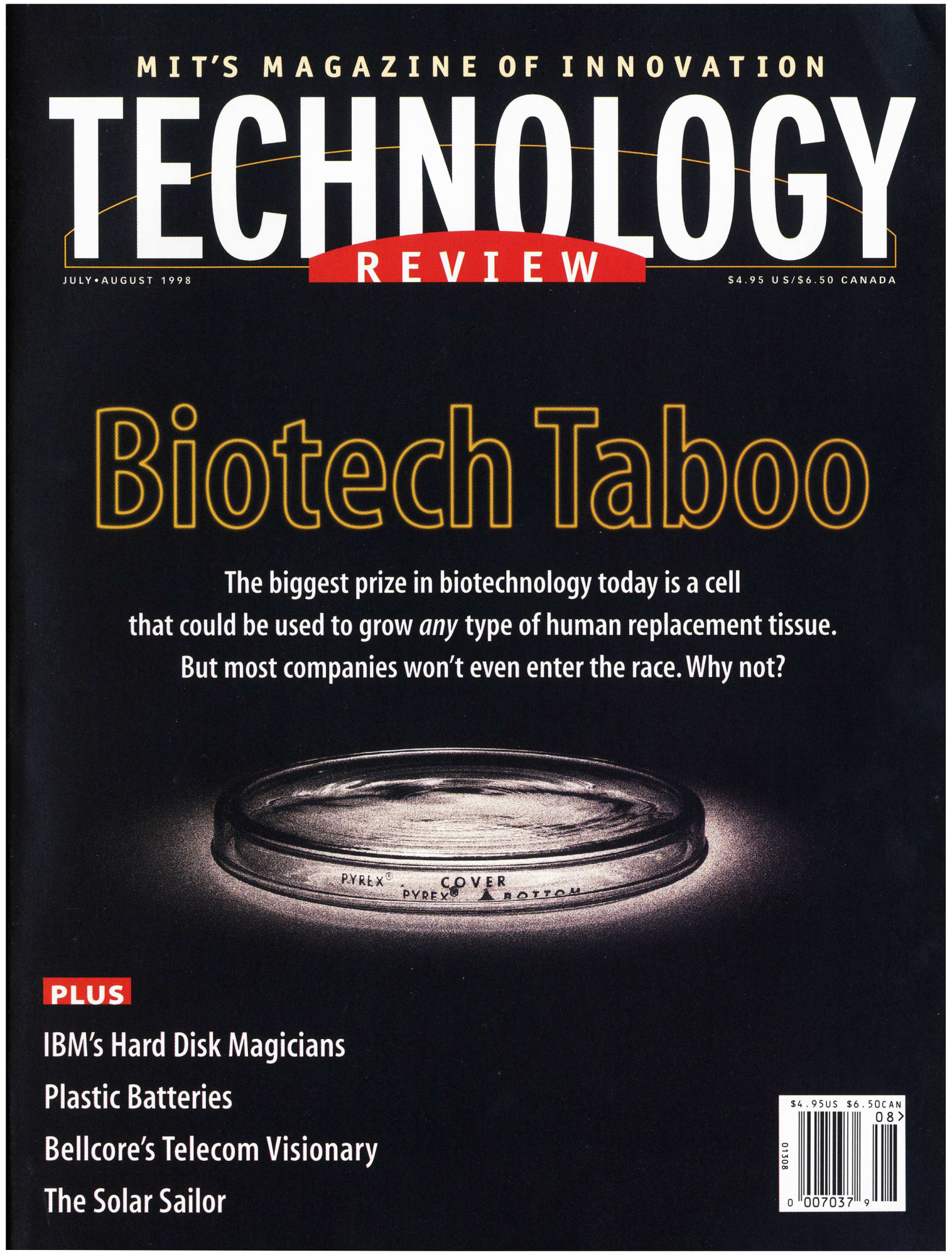
I have covered embryonic stem cells since the beginning— even a little bit before the beginning. Here at MIT Technology Review, we broke the story of the quest to isolate these cells, carried out under the looming threat of opposition from anti-abortion campaigners. Our July/August 1998 cover, “Biotech Taboo,” set the mood with a picture of a petri dish gleaming in the darkness.
“If awards were given for the most intriguing, controversial, and hush-hush of scientific pursuits,” I wrote, “the search for the embryonic stem cell would likely sweep the categories.” It was the search for a tabula rasa cell, we told readers—one able to give rise to any other type in the human body. The embryonic stem cell was a potential “factory in a dish” that could give scientists for the first time “the ability to grow human tissue at will.” And it was taboo because the cells existed only in early-stage human embryos, which could be obtained from IVF clinics but had to be destroyed in order to isolate the cells.
A few months after our report, the scientific race reached its conclusion. That November, James Thomson at the University of Wisconsin reported he’d captured stem cells from five embryos and was keeping these cells alive, and multiplying, in his lab.
Thomson’s paper, a succinct three-pager in the journal Science, contained a sketch of how he thought stem cells would become a medical technology. Where organs or cells from cadavers are in short supply, he predicted, stem cells “will provide a potentially limitless source of cells for drug discovery and transplantation medicine,” in particular by permitting “standardized production” of specialist cell types like beating heart cells or glucose-sensing beta cells. He noted that some diseases, specifically type 1 diabetes and Parkinson’s, result from “the death or dysfunction of just one or a few cell types.” If those specific cells could be replaced, it would mean “life-long treatment.”
That vision—that the mother of all cells could replace any tissue, or even regrow organs—is what electrified a generation of researchers. “That was the closest thing to magic that I have encountered. It’s a cell that keeps dividing and makes anything. If you are a cell biologist, that is the grail,” says Jeanne Loring, a professor emerita at the Scripps Research Institute and cofounder of Aspen Neuroscience, a company that plans to treat Parkinson’s disease with a transplant of dopamine-making cells. “The problem is, how do you make them into the precise cell type that you want?” What’s more, if stem cells are allowed to multiply in the lab, they can accumulate mutations, posing potential cancer risks: “That is the dark part of the magic.”
Political test
The stem-cell concept would shortly face a defining test—but it was political, not scientific. Because they’d been plucked from tiny, but living, IVF embryos, destroying them in the process, the discovery was met with outrage from the Catholic Church and other religious organizations in the US.
Two years after Thomson’s paper, George W. Bush was elected president. Now Christian conservatives had a line into the White House, and they wanted federal funding for the research on the cells blocked. Scientists, aided by patient advocates, reacted with an overwhelming lobbying campaign. Yes to cures, they rallied. “I love stem cells,” read the bumper stickers.
That equation—stem cells equals cures—made the breakthroughs seem closer than they really were. Martin Pera, editor in chief of Stem Cell Reports, an academic journal, was part of the push: in an editorial that year, for example, he wrote that treatments would be realized “soon,” if only the government and charities would fund the science. “It was all in our imagination at the time,” Pera told me when I saw him at the ISSCR meeting. “Because all we had were undifferentiated stem cells.”
Timothy Caulfield, a health law professor at the University of Alberta, would later analyze news articles and determine that scientists consistently made “authoritative statements” with “unrealistic timelines” for when cures would come. “I don’t blame the researchers,” he says. “There is a microphone in front of them, and five or 10 years is close enough yet far enough away. You have to make it exciting, revolutionary. If not, the money is going somewhere else.”
But the public believed these time frames—as well as the story that only a lack of funding stood in the way of cures. So after the US introduced some limits on stem-cell research (allowing research funding on only a few supplies of the cells), patient groups struck back. In California, a 2004 ballot initiative, Proposition 71, established the California Institute of Regenerative Medicine. It made stem-cell research a “constitutional right” in the state and allotted $3 billion in tax funds for research over 10 years. By that time, lobbyists predicted, the initiative would pay for itself twice over through a bonanza of jobs and cures. Just treating type 1 diabetes (“in year six,” according to a projection) would save $122 billion in insulin and other costs. One TV ad said stem cells would cure “a million people with Parkinson’s.”
None of those cures has reached the market yet. And many of the patient advocates from those years, some of whom hoped stem cells would save them, are now dead: Jenifer Estess, David Ames, the actor Christopher Reeve, and Jordan Klein. The last was the son of Bob Klein, the California real estate entrepreneur who’d put Prop 71 into motion. After Jordan died from complications of type 1 diabetes in 2016, age 26, his father blamed political delays, according to the Long Beach Business Journal. “My youngest son died. If they hadn’t held it up in DC, he would be alive,” Klein told the publication.
“There was this dystopian-versus-utopian view of stem cells in the early 2000s.”
-Timothy Caulfield
The belief in stem-cell cures had become entrenched. To people like Klein, it was political meddling that was delaying them. “There was this dystopian-versus-utopian view of stem cells in the early 2000s,” says Caulfield. “You had people saying it’s unethical or immoral or shouldn’t be allowed. The research community, and I was part of it, had to push back and say this is an exciting area and we are going to save lives. And all this language has survived.” The clearest evidence? Fly-by-night medical clinics that started cashing in on the hype, advertising stem-cell cures for autism, migraines, and multiple sclerosis—a phenomenon Caulfied calls “scienceploitation.” For many years, any Google search for stem cells would return ads from shady clinics offering to treat just about anything, usually with cells collected from blood or fat tissue.
I learned how pervasive the phenomenon is this spring when an elderly acquaintance revealed she’d paid over $7,000 in cash for an injection of supposed stem cells drawn from her bones in the hopes of treating a painful knee. Of course, it likely didn’t do anything. She could have saved her money had she read a pamphlet from the ISSCR called “Guide to Stem Cell Treatments.” Despite its title, which sounds like a product glossary, it’s a lengthy warning about scam clinics, explaining that essentially any stem-cell treatment you see advertised today is a fake.
That’s because, in reality, nothing could make stem cells move faster than the speed of science. “When the promise of stem cells reached the public consciousness … there was the idea that stem cells are themselves a magic cure, even though that is ridiculous,” says Arnold Kriegstein, a professor at the University of California, San Francisco. “The true promise was not that the stem cells would do this, but that they were the starting point for the cells you wanted. And that is never simple. That is painstaking and slow. That is science—it’s laborious and takes time.”
Delayed promise
Stem-cell research is no longer as political as it once was. That’s partly because by 2006, scientists had determined how to convert any cell, like a bit of skin, into something like an embryonic stem cell. Such “induced” stem cells are largely identical to those from embryos, and without the ethical hangover. But whichever type of stem cell researchers choose, using them to manufacture mature, specialized cells (the kind you’d want for transplant) turned out to be more difficult than most expected.
While the cookbook process can be successful, it is extraordinarily difficult to hit on a correct recipe. For instance, the scientist Douglas Melton, who has two children with type 1 diabetes and who developed the Vertex treatment that’s now in testing, spent close to 15 years before he was able to produce “functional” pancreatic cells able to respond to glucose and make insulin when transplanted into a mouse. “That problem took much longer than I expected—I told my wife it would take five years,” Melton recounted to a Harvard publication in 2021.
What’s more, maturing into a wanted cell type can take stem cells as long in a lab as it does during an actual pregnancy—sometimes six or seven months. That’s been a significant obstacle to trying out new ideas, since each new test means a further long delay. “I was optimistic, but when you do the experiment, it can take 200 days,” says Hanae Lahlou, a principal scientist at Mass Eye and Ear, one of Harvard’s teaching hospitals. She was part of a project that tried using transplants to repair the hearing of guinea pigs. They hoped the engrafted cells would grow into new auditory hairs, but they never quite did. Now Lahlou is trying speedier genetic techniques rather than cell transplants. “At some point I didn’t see it as a therapeutic tool,” she says. “If you ask patients, they want a drug.”
Making cells isn’t cheap, either. Just a gram of their favorite growth factor costs $750,000. Add to that the regulatory barriers that face any untested approach, and it’s clear why biotechnology companies’ work with stem cells has been fitful. Geron, which once controlled a patent on embryonic stem cells and launched the first human test of a treatment created from them in 2010, canceled the study a year later. Now it works on cancer drugs and no longer mentions embryonic stem cells on its website. Another stem-cell company, Sana, has seen its stock value droop since its 2021 IPO and last year laid off a team trying to create heart muscle to treat cardiac disease.
Early stage trials
High costs and technical difficulties aren’t unusual in the biotech world, and there is still a resilient cadre of investors and scientists who believe that stem-cell therapies are worth the risk. Today, stem-cell researchers say the increasing number of new clinical trials—about 15 are launching each year—is a sign the field may be close to a turning point. Transplants of lab-made retina cells (the approach tested most often so far) can’t be said to improve eyesight yet, but there is evidence from the initial handful of patients that the cells are doing something. According to a survey published last year, more than 3,000 patients have received transplants generated from induced or embryonic stem cells in around 90 studies, though all of these tests remain in their initial phases.
Yet Loring is hopeful that one of these tests will soon lead to striking, incontrovertible proof that treatments crafted from embryonic stem cells can cure disease. “It could be the tipping point,” she says. “And I do think we need that moment.”
Epilepsy treatment
During the three days I spent at the gathering of stem-cell researchers, one study stood out to me as looking like the big breakthrough this field needs. It’s a new trial being run by a biotech called Neurona Therapeutics, in San Francisco, which a year ago transplanted lab-made “inhibitory interneurons” deep into the brains of two people whose intractable epilepsy wasn’t responding to ordinary drugs. The bet is that these added cells will each form thousands of connections and quiet the malfunctioning brain networks that cause seizures.
During the meeting, Neurona announced that both patients have seen a 90%-plus reduction in seizures. In the case of one 26-year-old-man, that’s down from a debilitating 32 seizures a month. If the data holds up, it could mean the cell transplant is as effective as the most drastic treatment available for epilepsy today, which is surgical removal of part of the temporal lobe. But it wouldn’t have the side effects of getting part of your brain removed, like lost memories and vision.
“There’s a lot of enthusiasm. This could be the first cell therapy for epilepsy,” says Kriegstein, the professor at the University of California, San Francisco, who is also an adviser to Neurona and its cofounder. Kriegstein told me he doesn’t think 25 years is a long time for this type of therapy to emerge. Instead, he counters, it’s “actually kind of fast.”
Doctors had experimented with neuron grafts before—one company tried using cells from pigs. But it was Cory Nicholas, a postdoctoral fellow in Kriegstein’s lab, who first determined, in 2013, how embryonic stem cells might be coaxed towards forming human interneurons in large quantities. What followed was what Kriegstein calls a series of “rational, systematic” steps over a decade to improve that recipe, run tests on animals, and win approval to start a human trial. Most of that work was done at Neurona, which has raised over $160 million and where Nicholas is CEO.
“Obviously, this wouldn’t be possible without embryonic [or induced] stem cells,” says Kriegstein.
With only two patients treated, Neurona’s results remain anecdotal. But there’s a chance it’s an actual cure. That’s because the transplanted cells are likely still forming connections, and their effect may increase with time, possibly preventing seizures altogether. “It did seem like a pipe dream at first, but being able to make these cells in unlimited numbers is what let us try. Now we have patients who’ve been helped. It’s really quite amazing when you think about it,” says Kriegstein. “We are in the clinic. Cells are in patients, and we are going to see now how well they work. We are right at the point that the clinical trials will give us some clues. Was it just hype, or is it real?”
News
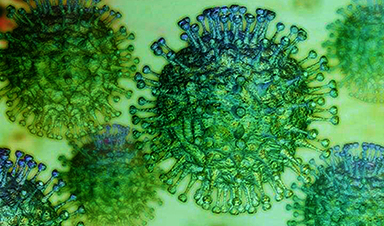
These two viruses may become the next public health threats, scientists say
Two emerging pathogens with animal origins—influenza D virus and canine coronavirus—have so far been quietly flying under the radar, but researchers warn conditions are ripe for the viruses to spread more widely among humans. [...]
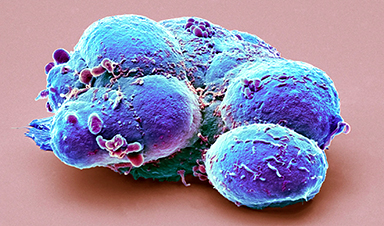
COVID-19 viral fragments shown to target and kill specific immune cells
COVID-19 viral fragments shown to target and kill specific immune cells in UCLA-led study Clues about extreme cases and omicron’s effects come from a cross-disciplinary international research team New research shows that after the [...]
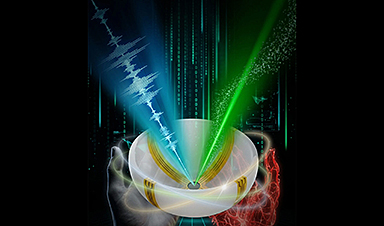
Smaller Than a Grain of Salt: Engineers Create the World’s Tiniest Wireless Brain Implant
A salt-grain-sized neural implant can record and transmit brain activity wirelessly for extended periods. Researchers at Cornell University, working with collaborators, have created an extremely small neural implant that can sit on a grain of [...]
Scientists Develop a New Way To See Inside the Human Body Using 3D Color Imaging
A newly developed imaging method blends ultrasound and photoacoustics to capture both tissue structure and blood-vessel function in 3D. By blending two powerful imaging methods, researchers from Caltech and USC have developed a new way to [...]
Brain waves could help paralyzed patients move again
People with spinal cord injuries often lose the ability to move their arms or legs. In many cases, the nerves in the limbs remain healthy, and the brain continues to function normally. The loss of [...]
Scientists Discover a New “Cleanup Hub” Inside the Human Brain
A newly identified lymphatic drainage pathway along the middle meningeal artery reveals how the human brain clears waste. How does the brain clear away waste? This task is handled by the brain’s lymphatic drainage [...]
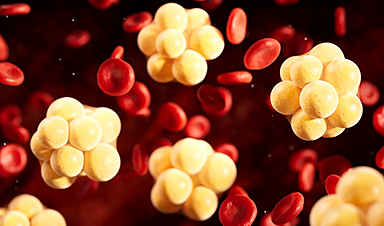
New Drug Slashes Dangerous Blood Fats by Nearly 40% in First Human Trial
Scientists have found a way to fine-tune a central fat-control pathway in the liver, reducing harmful blood triglycerides while preserving beneficial cholesterol functions. When we eat, the body turns surplus calories into molecules called [...]
A Simple Brain Scan May Help Restore Movement After Paralysis
A brain cap and smart algorithms may one day help paralyzed patients turn thought into movement—no surgery required. People with spinal cord injuries often experience partial or complete loss of movement in their arms [...]
Plant Discovery Could Transform How Medicines Are Made
Scientists have uncovered an unexpected way plants make powerful chemicals, revealing hidden biological connections that could transform how medicines are discovered and produced. Plants produce protective chemicals called alkaloids as part of their natural [...]
Scientists Develop IV Therapy That Repairs the Brain After Stroke
New nanomaterial passes the blood-brain barrier to reduce damaging inflammation after the most common form of stroke. When someone experiences a stroke, doctors must quickly restore blood flow to the brain to prevent death. [...]
Analyzing Darwin’s specimens without opening 200-year-old jars
Scientists have successfully analyzed Charles Darwin's original specimens from his HMS Beagle voyage (1831 to 1836) to the Galapagos Islands. Remarkably, the specimens have been analyzed without opening their 200-year-old preservation jars. Examining 46 [...]
Scientists discover natural ‘brake’ that could stop harmful inflammation
Researchers at University College London (UCL) have uncovered a key mechanism that helps the body switch off inflammation—a breakthrough that could lead to new treatments for chronic diseases affecting millions worldwide. Inflammation is the [...]
A Forgotten Molecule Could Revive Failing Antifungal Drugs and Save Millions of Lives
Scientists have uncovered a way to make existing antifungal drugs work again against deadly, drug-resistant fungi. Fungal infections claim millions of lives worldwide each year, and current medical treatments are failing to keep pace. [...]
Scientists Trap Thyme’s Healing Power in Tiny Capsules
A new micro-encapsulation breakthrough could turn thyme’s powerful health benefits into safer, smarter nanodoses. Thyme extract is often praised for its wide range of health benefits, giving it a reputation as a natural medicinal [...]
Scientists Develop Spray-On Powder That Instantly Seals Life-Threatening Wounds
KAIST scientists have created a fast-acting, stable powder hemostat that stops bleeding in one second and could significantly improve survival in combat and emergency medicine. Severe blood loss remains the primary cause of death from [...]
Oceans Are Struggling To Absorb Carbon As Microplastics Flood Their Waters
New research points to an unexpected way plastic pollution may be influencing Earth’s climate system. A recent study suggests that microscopic plastic pollution is reducing the ocean’s capacity to take in carbon dioxide, a [...]